- Received January 25, 2021
- Accepted February 23, 2021
- Publication April 03, 2021
- Visibility 10 Views
- Downloads 3 Downloads
- DOI 10.18231/j.achr.2021.002
-
CrossMark
- Citation
Spectrum of pap smear cytology in women presenting in a tertiary care center in north India-a two year study
- Author Details:
-
Honey Bhasker Sharma
-
Megha Bansal *
-
Nikhilesh Kumar
-
Monika Gupta
Introduction
Cervical cancer is an increasing health problem and an important cause of mortality in women worldwide. The incidence of cervical cancer arises worldwide. The difference in incidence between developing and developed countries is large. In developing countries like India, the burden of cervical cancer is still high. According to the world cancer statistics, >80% of all cancer cases are found in developing and low resource countries, because of a lack of awareness and difficulty in running cytology based screening programmes.[1]
More than one fifth of all cervical cancer deaths occur in India.[2] If diagnosed and treated early morbidity may be reduced by 70% and mortality by 80%.The papanicolaou test also known as Pap test, Pap smears, cervical smear or smear test is a screening method used to detect potentially precancerous and cancerous processes in the cervix. Greek doctor Georgios Papanikolaou invented this test and it was named after him.[3]
Pap smear is pivotal in cervical cancer screening in developing countires. It also identifies various inflammatory, infective, benign and malignant pathologies at the earliest.[4]
It is a simple, safe and effective test to detect premalignant and malignant lesions of the cervix at an early age.[5] It is recommended that females who are having sexual exposure should undergo regular Pap smear testing.[6] It should be a continuous process in order to prevent people dropping out for follow up visits and treatment procedure.[7]
Pap smear testing is strongly recommended in women in INDIA for early detection and treatment of premalignant, malignant and inflammatory conditions.[8]
First Bethesda system of cervical smear reporting was developed in 1988 and a two tier system i.e low grade squamous intraepithelial lesions (LSIL) and high grade squamous intraepithelial lesion (HSIL) was introduced and also used adequacy criteria alongwith human papilloma virus related preinvasive changes in the cervical epithelium.[9]
Our study aims to present the pap smear results based on Bethesda system2014 by evaluating the benign, infective and precancerous lesions in women presenting to our tertiary care center.
Subjects and Methods
This study was conducted at a tertiary care institute of Lucknow over a period of two years from June 2016 to June 2018 and a total 0f 450 patients were included, who reported to TSM Hospital Lucknow with chief complaints of vaginal discharge , menstrual irregularities, pelvic pain and dysparenuria.
Pregnant patients, patients who were been treated before for frank carcinoma cervix and patients who were bleeding at the time of examination were excluded from the study.
Cervical smears were taken using conventional method of cervical cytology by using pap kit (endocervical brush, Ayres spatula and cotton swab). Smears were fixed immediately in 95% ethylalcohol and stained by Pap staining. Smears were reported as per the Bethesda system 2014.
Results
Out of 450 cases, 411 cases (91.3%) were reported as negative for intraepithelial lesion/malignancy, 31 cases (6.9%) were showing epithelial cell abnormality and 8 cases (1.7%) were unsatisfactory. In negative for intraepithelial lesion cases, 4 cases (0.9%) were atrophic smears, 357 cases (79.3%) were inflammatory and the remaining 50 cases (11.1%) were showing no other changes. In inflammatory cases 53 cases (11.7%) showed presence of microorganisms. 31 cases showing an intraepithelial lesion - 15 cases(3.3%) were ASCUS, 3 cases (0.6%) were AGUS, 6 cases (1.2%) were LSI , 4 cases (0.8%) of ASC-H,2 cases(0.4%) were HSIL and one case (0.2%) of squamous cell carcinoma cervix as shown in [Table 1].
|
Pap Smear Diagnosis |
Number of patients |
Percentage of patients% |
|
1.Unsatisfactory |
08 |
1.7 |
|
2.NILM |
411 |
91.3 |
|
A.Inflammatory |
357 |
79.3 |
|
a.Nonspecific |
308 |
67.5 |
|
b.Trichomonas vaginalis |
03 |
0.67 |
|
c.Candida |
16 |
3.5 |
|
d.Bacterial vaginosis |
34 |
7.5 |
|
B.Atrophy |
04 |
0.9 |
|
C. No other changes |
50 |
11.1 |
|
3.Epithelial cell abnormality |
31 |
6.9 |
|
a.ASCUS |
15 |
3.30 |
|
b.AGUS |
03 |
0.6 |
|
c.LSIL |
06 |
1.3 |
|
d.HSIL |
02 |
0.4 |
|
e.ASC-H |
04 |
0.8 |
|
f.SCC |
01 |
0.2 |
Most common age group showing epithelial cell abnormality was 41-60 yrs of age. The examination of 31 abnormal smears reveal 15 cases (3.3%) of ASCUS with maximum number in age group 51-60 years, AGUS- 3 cases maximum in the ages 31-40 yrs, LSIL -6 cases maximum in the age range 41-50 yrs. HSIL -2 cases maximum in age range 41-50 yrs. Squamous cell carcinoma cervix only one case of age 70 years as shown in table 2. In our study mean age of ASCUS & LSIL was 51 years, 59 yrs for ASC-H, 50 yrs for HSIL & 70 yrs for ca cervix.
|
Epitheilal Cell Abnormality |
Age <20yrs |
Age 21-30yrs |
Age 31-40yrs |
Age 41-50yrs |
Age 51-60yrs |
Age 61-70yrs |
Total |
|
ASCUS |
- |
- |
01 |
05 |
08 |
01 |
15(48.4%) |
|
AGUS |
- |
- |
02 |
01 |
- |
- |
03(9.6%) |
|
ASC-H |
- |
- |
- |
- |
03 |
01 |
04(13%) |
|
LSIL |
- |
01 |
01 |
03 |
- |
01 |
06(19.3%) |
|
HSIL |
- |
- |
- |
02 |
- |
- |
02(6.4%) |
|
SCC |
- |
- |
- |
- |
- |
01 |
01(3.3%) |
Microscopy of inflammatory smears reveal bacterial vaginosis, Trichomonas, Candidiasis, and other non specific infections as shown below in [Table 3].
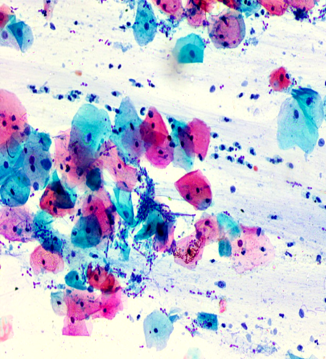
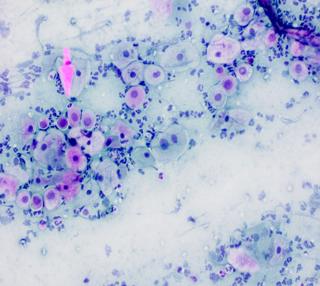
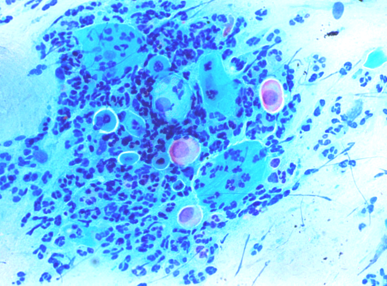
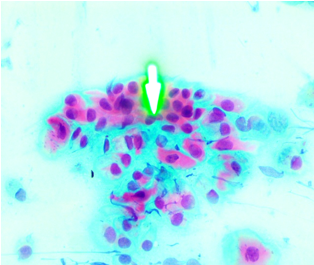
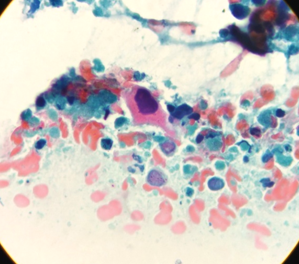
[Figure 1] shows candidial hyphae and spores.[Figure 2] shows bacterial vaginosis with clue cells. [Figure 3] shows ASCUS, [Figure 4] shows LSIL.[Figure 5], [Figure 6] shows squamous cell carcinoma cervix.
|
Inflammatory smear |
Age <20yrs |
Age 21-30yrs |
Age 31-40yrs |
Age 41-50yrs |
Age 51—60yrs |
Age 61-70yrs |
Total |
|
Non specific inflamation |
05 |
113 |
110 |
60 |
10 |
06 |
304(85.3%) |
|
Bacterial vaginosis |
02 |
12 |
13 |
07 |
- |
- |
34(9.4%) |
|
Trichomonas vaginalis |
01 |
01 |
01 |
- |
- |
- |
03(0.83%) |
|
Candida |
- |
03 |
07 |
05 |
01 |
- |
16(4.43%) |

Discussion
In a study done by Singh K and Singh A in 2015 they revealed negative for intraepithelial lesions in 156 cases (83.9%) cases and epithelial cell abnormality in 30(16%) cases. [10] In our study we found negative for intraepithelial lesions in 411 cases (91.3%) and epithelial cell abnormalities in 31cases (6.8%).
In a study done by Sachan P, Singh M, Patel M, Sachan R in 2018 they found ASCUS in 2.9% of screened women, LSIL in 5.09%, and HSIL in 0.48% cases.[11] In their study Lakshmi P et al found ASCUS in 5 cases (2.5%), LSIL in 15 cases(7.5%), and HSIL in 1 case(6%) cases [12] In our study we found ASCUS in 15cases (3.3%), LSIL in 6 cases(1.3%), HSIL in 2 cases (0.4%) and AGUS in 3cases (0.6%), ASC-H in 4 cases (0.8%) and SCC cervix in 1 case (0.2%) as shown in [Table 4].
|
Epithelial Abnormality |
Sachan P et al(2018) [11] |
Lakshmi P et al [12] |
Present study |
|
ASCUS |
2.9% |
2.5% |
3.3% |
|
LSIL |
5.09% |
7.5% |
1.3% |
|
HSIL |
0.48% |
6% |
0.4% |
In a study done by Warpe B M et al in 2016 , nonspecific inflammation was found in 61.2%, candida infection in 0.8%, Trichomonas infection 7.35% , bacterial vaginosis in 12.24%.[13] Similar results were obtained in their study by Kalyani R et al in 2016. [14] Study done by Sethi PK et al in 2014 showed similar results.[15] Pudasaini S, et al in 2015 found Bacterial vaginosis (5.3%) was commonest among organisms in their study which was similar to our study. [16]
In the study done by Rawat Kiran et al in 2016 mean age of patients with LSIL was 39.1years and those of ASC-H, HSIL & Carcinoma cervix were 54, 51.1 and 64.6 years respectively. [17] While in our study mean age of LSIL was 51 years, 59yrs for ASC-H, 50yrs for HSIL & 70yrs for carcinoma cervix.
Conclusion
Premalignant and malignant lesions of cervix are common and can be diagnosed early by conventional PAP smears. Conventional pap smears are essential not only to diagnose premalignant lesions but also to identify the infectious etiologies and guide proper treatment. Cervical cancer commonly occurs in women between ages 60and 70 years and its precursor lesion occurs 10-20 years earlier. Therefore it is recommended that women should have atleast one pap smear test before the age of 45 years. Thus, we have to strengthen our health services to spread cervical cancer screening programs, educate and motivate women to visit the hospital for cancer screening.
Conflicts of Interest
All contributing authors declare no conflicts of interest.
Source of Funding
None.
References
- J Ferlay, I Soerjomataram, R Dikshit, S Eser, C Mathers, M Rebelo. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015. [Google Scholar] [Crossref]
- L Bruni, L Barrionuevo-Rosas, G Albero, M Aldea, B Serrano, S Valencia. ICO Information Center on HPV and Cancer(HPV Information Centre) Human Papillomavirus and Related Diseases Reports.Last accessed on. 2015. [Google Scholar]
- Pap Smear. By Healthline medical review team. . [Google Scholar]
- PG Ghimire, DBC Rawat, K Sinha, K Jahan, R Shrestha. Spectrum of cytological patterns in cervical PAP smears in a tertiary care center of Western region of Nepal. Nepal J Med Sciences 2019. [Google Scholar] [Crossref]
- G Mudassir, M Abid, H Naveed. The Taliban Conundrum. J Rawalpindi Med Coll 2017. [Google Scholar] [Crossref]
- L Padmom, B Devi, K Sapru. Cervical smears-study done in a tertiary care hospital. J Evol Med Dent Sci 2019. [Google Scholar] [Crossref]
- S Arul Anne Rose. Pattern of Pap smear cytology:our experience.International journal of reproduction, contraception. Obstet Gynecol 2016. [Google Scholar]
- SS Biradar, SP Rashmi. An Analysis of Various Cytopathological Patterns on Papanicolaou smears-Cervical Cytology: A Study in Tertiary Care Hospital. Int J Clin Diagn Pathol 2020. [Google Scholar] [Crossref]
- R Nayar, DC Wilbur. The Bethesda System for Reporting Cervical Cytology:Definitions, Criteria, and Explanatory Notes. 3rd Edn. 2015. [Google Scholar]
- K Singh, A Singh. A Clinicopatholoical correlation of pap smear findings in gynecological cases: A retrospective study. Int J Sci Res 2015. [Google Scholar]
- R Sachan, PL Sachan, M Singh, ML Patel. A Study on Cervical Cancer Screening Using Pap Smear Test and Clinical Correlation. Asia-Pacific J Oncol Nurs 2018. [Google Scholar] [Crossref]
- P Lakshmi, S Gouri. Study and Analysis of Two Hundred Cervical Pap smears in our Hospital. Int J Contemp Med Res 2016. [Google Scholar]
- B Warpe, S Warpe, S Sawant. An institutional based Cervical PAP smear study, correlation with clinical findings and histology in the Konkarn region of Maharashtra state, India. Walawalkar Int Med J 2016. [Google Scholar]
- R Kalyani, N Sharief, S Shariff. A study of PAP smear in Tertiary Hospital in South India. J Cancer Biol 2016. [Google Scholar]
- P K Sethi, A Singh, H Kaur, N Sood. Trends in cervical cytology of conventional Papanicolaou smears according to revised Bethesa system: A study of 638 cases. IJRRMS 2014. [Google Scholar]
- S Pudasaini, KBR Prasad, SK Rauniyar, R Pathak, K Pande, S Koirala. Cervical pap smear- A prospective study in a tertiary hospital. J Pathol Nepal 2015. [Google Scholar] [Crossref]
- Kiran Rawat, Narendra Rawat, Navgeet Mathur, Medha Mathur, Nitesh Chauhan, Rajat Tinna, Rahul Kakkar. A study of cytological pattern of cervical papanicolaou smears in western Rajasthan, India. International Journal of Reproduction, Contraception, Obstetrics and Gynecology 2016. [Google Scholar] [Crossref]
