- Visibility 132 Views
- Downloads 42 Downloads
- Permissions
- DOI 10.18231/j.achr.2024.038
-
CrossMark
- Citation
Fungal bezoar of bladder in type 2 diabetic mellitus patient: A case report
Abstract
A 54 year male, post operated case of bypass surgery presented to a Urologist with acute retention of urine. Patient was relieved by catheterization and bladder irrigation. WBC’s and RBC’s were increased in Urine. Cystoscopy revealed fungal balls in the bladder which on histopathological examination showed aseptate hyphae and spores. Patient was managed by systemic voriconazole and diluted povidone iodine bladder wash. Predisposing factors were diabetes mellitus and dyslipidemia. This case stresses the importance of considering isolated fungal urinary infections in predisposed individuals.
Introduction
Fungal bezoar in urinary bladder is a rare pathological entity, of which less than 20 previous cases have been described in the literature since the first case was reported in 1961.[1] Fungal bezoars are frequent in immunocompromised individual, hospitalized patients with multiple comorbidities and those with severe illness requiring admission to intensive care units. [2] Here, we present a case of Urinary bladder fungal balls without disseminated.
Case Presentation
In our case, we will discuss a case of urinary fungal bezoar infection that was severe enough to cause acute retention of urine, render the patient anuric. Our patient is a 54 year male, he had undergone bypass surgery two and half months before. Since his surgery, the patient was hospitalized for a long period i.e. for 10 -12 days and received broad spectrum antibiotics. The patient was kept on urinary catheter as it was difficult for him to mobilize. A week after his discharge from hospital, the patient felt bladder fullness and bilateral flank pain with anuria. Patient was relieved by catheterization and bladder irrigation.
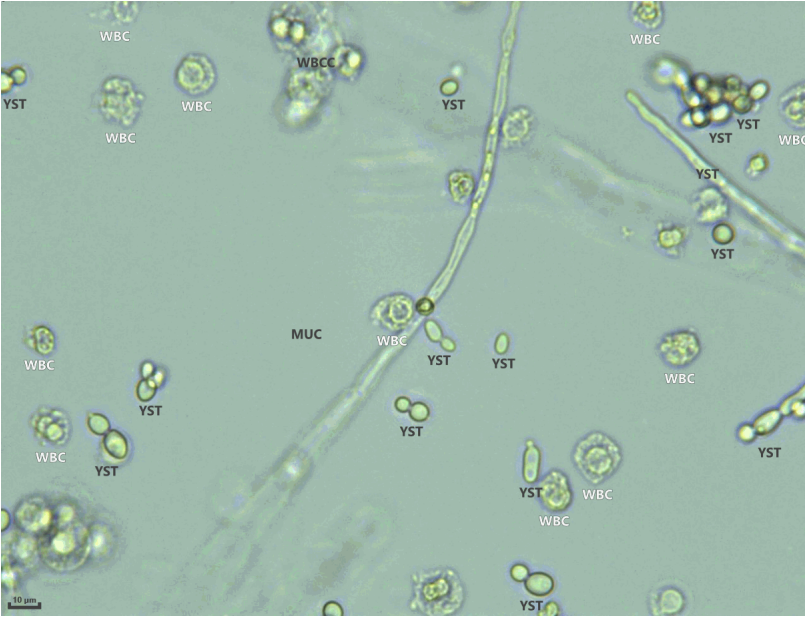
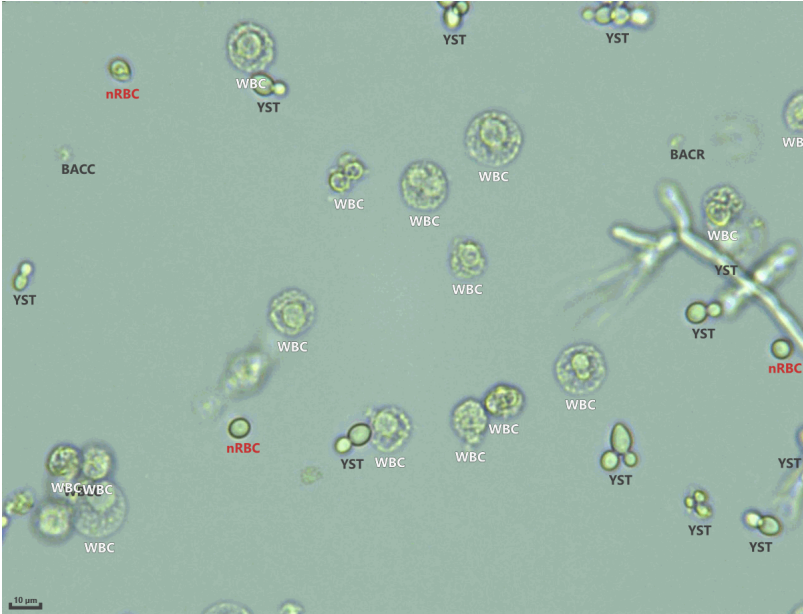

His urine routine microscopy on Transasia Laura XL Fully automated Urine analyzer reveals increased pus cells 194/hpf and RBC’s 27/hpf. Fungal hyphae and yeast forms were seen on microscopy ([Figure 1], [Figure 2]).
We also received urine with flakes for histopathological examination. Grossly multiple dirty white color flakes altogether measuring 2.0 x 1.5 x 0.5 cm received. Microscopic examination shows necrosed tissue with dense mixed inflammatory cell exudate with many fungal colonies. These fungal colonies were aseptate hyphae and spores ([Figure 3])
Discussion
Fungal Urinary tract infections are more likely to develop in patients with predisposing factors such as Urinary catheterization, ICU stay, use of broad-spectrum antibiotics, diabetes and glucocorticoids therapy. [3], [4], [5] Fungal bezoars can be found anywhere in the urinary tract, and so its clinical presentation depends upon site of the bezoars. Urinary tract obstruction at renal pelvis or ureteric bezoars might elevate renal function test and hydronephrosis. In such cases surgical intervention such as nephrostomy or ureteric stenting is usually necessary.[6], [7] Previous case reports have shown fungal bezoars spreading to both pelvicalyceal systems causing bilateral renal obstruction at the level of renal pelvis and ureters leading to acute renal failure and anuria. [8], [9]
Unlike simple bacterial or fungal UTIs, the treatment of fungal bezoars may require local intervention in addition to systemic therapy with antifungals. Fungal balls could be also directly extracted using flexible ureteroscopy, cystoscopy, PCNL or by surgical exploration in more complicated cases. [10], [11] Urinary microscopy and histopathological examination lead to definitive diagnosis. So as proper treatment of this condition would be essence to prevent further complications and to avoid the need for more invasive measures.
Conclusion
Fungal infections of urinary tract even though rare should always be kept as differential diagnosis in patient of persistent UTI, especially in susceptible populations such as hospitalized patients, or one with comorbidities. Urine routine microscopy and histopathological examination play a key role in early diagnosis on fungal bezoars and prevention of further future complication.
Conflicts of Interest
The authors declare that they have no conflicts of Interest.
Source of Funding
None.
References
- Chisholm ER, Hutch J. Fungus ball (Candida albicans) formation in the bladder. J Urol. 1961;86(5):559-62. [Google Scholar]
- Kobayashi C, Fernandes O, Miranda K, Sousa ED, Silva M. Candiduria in hospital patients: a study prospective. Mycopathologia. 2004;158(1):48-52. [Google Scholar]
- Gharanfoli A, Mahmoudi E, Torabizadeh R, Katiraee F, Faraji S. Isolation, characterization, and molecular identification of Candida species from urinary tract infections. Curr Med Mycol. 2019;5(2):33-6. [Google Scholar]
- Odds F. Factors that predispose the host to candidosis. Candida and Candidosis. Bailliere Tindall. 1988. [Google Scholar]
- Achkar J, Fries B. Candida infections of the genitourinary tract. Clin Microbiol Rev. 2010;23(2):253-73. [Google Scholar]
- Merode NV, Pat J, Wolfhagen M, Dijkstra G. Successfully treated bilateral renal fungal balls with continuous anidulafulgin irrigation. Urol Case Rep. 2021;34. [Google Scholar] [Crossref]
- Das M, Pakshi R, Kalra S, Elumalai A, Theckumparampil N. Fungal Balls Mimicking Renal Calculi: A Zebra Among Horses. J Endourol Case Rep. 2019;5(4):167-70. [Google Scholar]
- Scerpella E, Alhalel R. An unusual cause of acute renal failure: bilateral ureteral obstruction due to Candida tropicalis fungus balls. Clin Infect Dis. 1994;18(3):440-2. [Google Scholar]
- Ku J, Kim M, Jeon Y, Lee N, Park Y. Urinary ascites and anuria caused by bilateral fungal balls in a premature infant. Arch Dis Child Fetal Neonatal Ed. 2004;89(1):92-3. [Google Scholar]
- Kittaweerat N, Attawettayanon W, Choorit T. Bilateral renal fungal bezoars in a preterm infant: case report and literature review. J Surg Case Rep. 2021. [Google Scholar] [Crossref]
- Comiter C, Mcdonald M, Minton J, Yalla S. Fungal bezoar and bladder rupture secondary to candida tropicalis. Urology. 1996;47(3):439-41. [Google Scholar]
How to Cite This Article
Vancouver
Hawaldar R, Khan SN. Fungal bezoar of bladder in type 2 diabetic mellitus patient: A case report [Internet]. IP Arch Cytol Histopathol Res. 2024 [cited 2025 Oct 21];9(3):169-171. Available from: https://doi.org/10.18231/j.achr.2024.038
APA
Hawaldar, R., Khan, S. N. (2024). Fungal bezoar of bladder in type 2 diabetic mellitus patient: A case report. IP Arch Cytol Histopathol Res, 9(3), 169-171. https://doi.org/10.18231/j.achr.2024.038
MLA
Hawaldar, Ranjana, Khan, Shana Nikhat. "Fungal bezoar of bladder in type 2 diabetic mellitus patient: A case report." IP Arch Cytol Histopathol Res, vol. 9, no. 3, 2024, pp. 169-171. https://doi.org/10.18231/j.achr.2024.038
Chicago
Hawaldar, R., Khan, S. N.. "Fungal bezoar of bladder in type 2 diabetic mellitus patient: A case report." IP Arch Cytol Histopathol Res 9, no. 3 (2024): 169-171. https://doi.org/10.18231/j.achr.2024.038
