
Print ISSN: 2581-5725
Online ISSN: 2456-9267
CODEN : IACHCL
IP Archives of Cytology and Histopathology Research (ACHR) open access, peer-reviewed quarterly journal publishing since 2016 and is published under the Khyati Education and Research Foundation (KERF), is registered as a non-profit society (under the society registration act, 1860), Government of India with the vision of various accredited vocational courses in healthcare, education, paramedical, yoga, publication, teaching and research activity, with the aim of faster and better dissemination of knowledge, we will be publishing the article more...Null
Author Details :
Volume : 4, Issue : 1, Year : 2019
Article Page : 75-81
https://doi.org/10.18231/2456-9267.2019.0013
Abstract
Introduction: Salivary gland lesions represent clinical and morphological diversity, which is a difficult task for histopathological interpretation. Classification of salivary glands lesions into non-neoplastic and neoplastic (benign and malignant tumors) is essentially based on histopathological aspect, which is important for management and predicting its prognosis.
Aims and Objectives: To study histomorphological (gross and microscopic) aspect of Salivary gland lesions. To classify salivary gland lesions for therapeutic implication. To study the different epidemiological pattern with particular references to age, gender, site and its incidence. To compare and observe the results of this study with other studies
Materials and Methods: This is a retrospective study done at Pathology Department, GMERS Medical College and Hospital, Sola, Ahmedabad. The specimens were fixed in 10% formalin, processed by paraffin embedding, stained with H & E and examined microscopically.
Results: Out of 66 cases, 22(33%) cases are non-neoplastic and 44(67%) cases are neoplastic. Among 44 neoplastic lesions, 42(95%) cases are benign and 02(5%) cases are malignant. Parotid gland is the most common and well known site for the all salivary glands lesions. Male female ratio was 3.4:1. The mean age found was 39.5 years with age scope of 3 to 72 years. Chronic sialadenitis is the most common non-neoplastic lesion. Most common benign tumor of salivary glands is pleomorphic adenoma followed by Warthin’s tumor. The mucoepidermoid carcinoma was only recognized malignant tumor followed by undifferentiated malignant tumor.
Conclusion: Owing to complex features exhibited by salivary gland lesions histopathological examination is the mainstay for final diagnosis and categorization for treatment and prognosis.
Keywords: Chronic sialadenitis, Pleomorphic adenoma, Mucoepidermoid carcinoma.
Salivary gland lesions represent clinical and morphological diversity, which is a difficult task for histopathological interpretation.[1]
The annual incidence ranging from 0.4 to 6.5 cases per lakh population. It accounts to less than 2-6.5% of all neoplasms of head and neck.[2]
Non-neoplastic lesions range from an inflammatory disorder of infectious, granulomatous, or autoimmune etiology to obstructive, developmental, and idiopathic disorders.[3]
In a series of 2632 salivary gland tumors reported by Eneroth, the incidence of malignancy was 17% for the parotid gland, 38% for the submandibular gland, and 44% for the palate.[4]
Benign tumors of the salivary glands usually can be distinguished from the high-grade malignant varieties on the basis of their clinical and gross characteristics.[4]
In addition, hybrid tumors, dedifferentiation and the propensity for some benign tumors to progress to malignancy can confound histopathological interpretation.[3]
There are almost 40 named epithelial tumours in the latest World Health Organization (WHO) classification it is evident that some tumours are very rare indeed and may be the subject of only a few case reports.[5]
Salivary gland tumors are 12 times more frequent in the parotid than in the submandibular gland.[2] Majority of Salivary gland tumours are of benign histology (80-85%), with pleomorphic adenoma being the most common, constituting 70% of benign tumours.[6]
Benign tumors may be present for months to several years before coming to clinical attention, while cancers more often come to attention promptly, there are no reliable criteria to differentiate benign from malignant lesions on clinical gronds, and histopathologic evaluation is essential.[7]
Due to a lack of long term follow up, screening and registration, risk factors and prevention are poorly known.
A diagnosis of salivary gland neoplasm must be considered in any patient who presents with a mass in the parotid or submandibular region or a sub mucosal mass in the oral cavity or pharynx.
Salivary gland tumors proved most difficult because its arise from or differentiate toward the same cell lines: epithelial (ductal or acinar) and abluminar (myoepithelial and/or basal cell) results in considerable overlap at all levels with these cells can undergo a variety of metaplastic changes.[4]
A preoperative sonography combined with FNAC, CT scan and MRI in some cases provides necessary clues prior to surgery. Although FNAC is a tool for pre-operative evaluation, Histopathology still remains the gold standard for final diagnosis.
Because of their rarity, individual clinicians are only infrequently required to manage these lesions and most cancers are managed in specialist centres.
This coupled with the degree of morphological diversity, makes this group of lesions one of the most interesting and challenging in the head and neck.[2]
The spectrum of salivary gland lesion is wide and the relative incidences of neoplastic versus non-neoplastic lesions are variable in different studies
Thus it is the responsibility of the pathologist to provide a precise diagnosis which can be used by the surgeon to group entities into broader prognostic groups relevant to management.
Aims and Objective
This is a retrospective study of total 66 cases conducted in the Pathology Department, GMERS medical college and hospital, Sola, Ahmadabad over a period of 5 years.
The source of data is from the biopsies of lesions of salivary glands that were received at the Pathology Department.
The hospital is a tertiary care government hospital offering histopathology services to the entire district. Demographic data (age, sex and site) were obtained from laboratory records derived from information provided on histopathology request forms.
The specimens were fixed in 10% formalin, processed by paraffin embedding, stained with H & E and examined microscopically.
Inclusion criteria:
Exclusion criteria: Inadequate and improperly fixed tissue biopsies.
In our study, total of 66 specimens of salivary gland specimens were reviewed. Out of 66 cases (Table 5), 22(33%) cases are non-neoplastic and 44(67%) cases are neoplastic. Among 44 neoplastic lesions, 42(95%) cases are benign and 02(5%) cases are malignant.
Chronic sialadenitis is the most common non-neoplastic lesion.
Most common benign tumor of salivary glands is Pleomorphic adenoma followed by Warthin’s tumor.
The mucoepidermoid carcinoma was the only recognized malignant tumor followed by undifferentiated malignant tumor.
The mean age found was 39.5 years with Affected patients are between 3 and 72 years age group. Predominantly males are affected.
Site Distribution
Table 1: Site of lesion
|
Site |
Parotid gland |
Submandibular gland |
Minor salivary gland |
Total |
|
Total No. (%) |
45 (68.18) |
21 (31.81) |
- |
66 (100) |
A maximum number of cases are seen in parotid gland constituting 45 cases (68.18%) followed by submandibular gland constituting 21 cases (31.81%) (Table 1).
Out of 45(68.18%) cases of parotid tumors, 7(15.5%) cases of non-neoplastic, 36(80%) cases of benign and 2(4.44%) cases of malignant lesions finding out.
Out of 21(31.81%) cases of Submandibular gland tumors, 15(71.42%) cases of non-neoplastic, 6(28.57%) cases of benign lesions finding out.
Age and Gender Distribution:
Salivary gland tumors studied were seen in the wide age group ranging from 3 years to 72 year. Most of the tumors were seen in middle age group with mean age of 39.5.
Overall, 77.27% of cases in the study were male with 22.72% female cases.
A maximum number of cases are seen in 21-30-year age group followed by 51-60-year age group. Table 2 shows male preponderance with M:F ratio 3.4:1.
Table 2: Age and Gender Distribution
|
Sex |
Number of cases (%) |
|
Males |
51 (77.27) |
|
Females |
15 (22.72) |
|
Total |
66 (100) |
Nature of salivary gland lesions: non-neoplastic lesions are 22 cases (33.33%) Neoplastic lesions are 44 cases (66.67%) (Table 3).
Table 3: Nature of salivary gland lesions
|
Nature |
Non-neoplastic |
Neoplastic |
Total |
|
Number of cases (%) |
22 (33.33) |
44 (66.67) |
66 (100) |
A maximum number of salivary gland neoplasms are benign neoplasms are 42 cases (95.45%) and malignant cases are 02 cases (4.54%) (Table 4).
Table 4: Incidence of salivary gland neoplasms
|
Nature |
Number of cases (%) |
|
Benign |
42 (95.45) |
|
Malignant |
02 (4.54) |
|
Total |
44 (100) |
Table 5: Morphological spectrum of salivary gland lesions
|
Lesions |
Number of cases (%) |
|
Acute suppurative inflammations |
01 (1.51) |
|
Chronic Submandibular sialadinitis |
01 (1.51) |
|
Chronic sclerosing sialadinitis |
06 (9.09) |
|
Chronic sialadinitis |
14 (21.21) |
|
Lymphoepithelial sialadinitis |
01 (1.51) |
|
Pleomprphic adenoma |
36 (54.54) |
|
Warthin tumors |
04 (6.06) |
|
Nerve sheth myxoma |
01 (1.51) |
|
Low grade Muco-epidermoid carcinoma |
01 (1.51) |
|
Poorly differentiated angiosarcoma |
01 (1.51) |
|
Total |
66 (100) |
In our study total, 66 cases of salivary gland lesions were processed over a period of 5 years.
Out of 66 cases, we found 33.33% cases of non-neoplastic lesions and among them 95% were of chronic sialadenitis with the peak incidence of 20 to 40 year and M:F ratio of 3.4:1. This study is similar to study done by Laishram et al[7] where in the nonneoplastic lesions 84.62% of cases were chronic sialadenitis with age incidence of 20-30 years and M:F ratio was 1.2:1.
In Neoplastic lesions benign tumors 95.45% predominate over the malignant tumours 4.54% as observed in the present study as well as in previous studies done by Ahmed et al[8] (86% benign and 14% malignant), Nagarkar et al[9](75% and 25%) and Ito et al[10] (67.5% and 32.5%).
From age wise distribution of neoplastic lesions, it was observed that benign lesion is seen in lower age group (Mean age 39.5 year) than malignant lesion (Mean age 46.5 year). This study is similar to study done by Thomas et al[11] (Benign-39 year and Malignant-47year), Ahmed et al[8] (35.7 year and 42.4 year) and Edda et al[12] (33.5 year and 43 year).
In the present study there is a male preponderance (M:F ratio of 3.4:1) in salivary lesions as in most of the studies by Ahmed et al[8] (M:F ratio 1.1:1), Mohd Ayub et al[13] (M:F ratio 2.25:1), and Iqbal MS et al[14] (M:F ratio 2:1), but female predominance in benign tumour (M:F ratio 1:1.36), which correlates with Edda et al[12] (M:F ratio 1:1.4), Mohd
Ayub et al[13] (M:F ratio 1:1.98), and Iqbal MS et al[14] (M:F ratio 1:1.53).
In our study parotid gland was the commonest site of neoplasia (68.18%) followed by submandibular gland (31.81%) which is accordant to other studies by Ahmed et al[6], Pablo et al,[13] Rewusuwan et al[14] and Bashir S et al.[15]
Pleomorphic adenoma was the most common tumor accounting for 54.54% of all tumors and 88.09% of all benign tumors. This correlates to the results of other series by Pablo et al[15] (67% of total tumor and 84% of total benign tumour), Nagarkar et al[9](52.77% of total tumor and 84.30% of total benign tumor) and Bashir S et al[16] (55% of total tumor and 89% of total benign tumor).
Acute suppurative sialadenitis is generally caused by Staphylococcus aureus, Streptococcus species, and gram-negative bacteria. Dehydration, malnutrition, immunosuppression, and sialolithiasis are predisposing factors.4 Once an abscess has formed, surgical drainage may be necessary. In our study we find 1.51% of acute suppurative siladenitis.
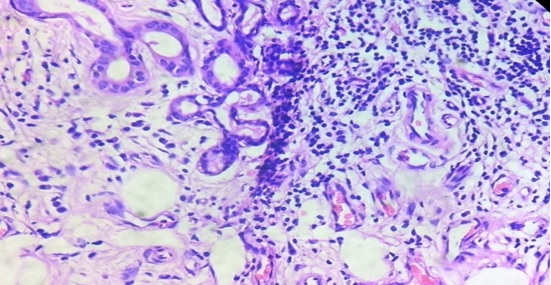
Chronic sialadenitis present in the form of mild lymphocytic infiltration of the major salivary gland unaccompanied by clinical symptoms. There are focal obstructive nature accompanied by various degrees of parenchymal atrophy, fibrosis, and microliths.[4] in our study we find 21.21% chronic siladenitis.
Kuttner tumor is a chronic sclerosing sialadenitis of the submandibular gland is characterized by a plasmacytic and lymphocytic periductal infiltrate with lobular architecture is preserved and obliterative phlebitis is frequently seen.[4] in our study we find 9.09% chronic siladenitis.
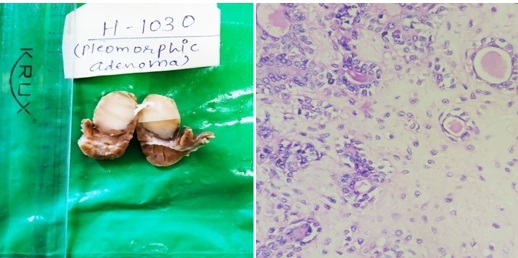
Pleomorphic adenoma: is the most common neoplasm of the salivary glands. It is most frequent in women in the fourth decade of life, but it can be seen in children and in elderly persons of either gender. It is approximately 10 times more common in the parotid than in the submandibular gland[4] Grossly, mostly present as rounded, well demarcated masses, cut surface is gray-white with myxoid and blue translucent areas of condroid. It may have bosselated surface and may grow to a large size but are usually between 2 and 5 cm. Histopathological feature shows both epithelial and mesenchymal differentiation. Epithelial component includes the well?formed ductal structures formed of inner epithelial and outer myoepithelial cells. The stroma may have a myxoid appearance and areas of clear-cut cartilaginous differentiation[4].(figure-3a) (figure-3b)
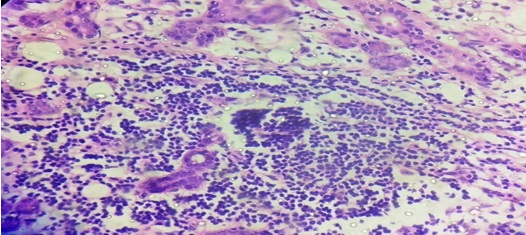
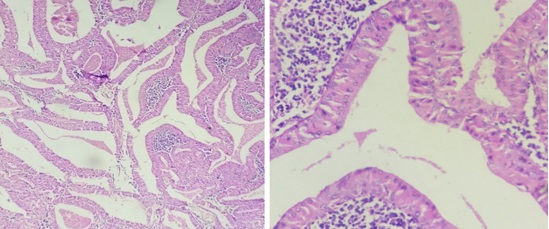
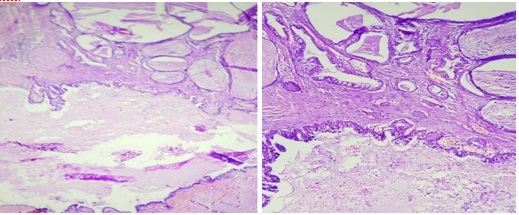
Warthin’s tumor: In our study the second most common benign tumor of salivary gland was Warthin’s tumor (9.52%), which was found only in the males and occurred exclusively in the parotid gland. Smoking habits are the main etiological factor for Warthin’s tumor[4]. Grossly, it appears as a lobulated brown mass and has a typical multicystic appearance, with fluid-filled spaces filled with dark brown fluid[4]. Microscopically, epithelial tall columnar (IHC?somatostatin) with basaloid oncocytic cells lining cysts form prominent papillae, the cystic spaces are filled with lymphoid stroma and few show lymphoid follicles. (Figure-4a) (Figure-4b).
Nerve sheth myxoma: microscopically there is prominent multinodularity with a fibrous border and presence of plumper, spindle like cells and distinct fascicular or plexiform arrengment.[4](Figure-5a) (Figure-5b)
Mucoepidermoid Carcinoma: The mucoepidermoid carcinoma was the only recognized epithelial malignant tumor in our study and it is most common form of primary malignant tumors of salivary gland. clinical couse and prognosis depend on histological grade. Microscopically, three main cell types can be identified: mucin-producing, squamous (epidermoid), and intermediate, which are present in variable proportions from tumor to tumor and can form sheets and nests with duct-like structures or cysts.[4] our case was low grade carcinoma showing cysting appearance grossly with predominant mucin secreting cells and squamous cells microscopically. The high-grade varieties are more solid and have a more infiltrative pattern of growth. In the high-grade tumors, squamous and intermediate predominate over the mucin-producing cells.[4](Figure-6a) (Figure-6b)
Poorly differentiated angiosarcoma: The most common locations are the skin, soft tissue, breast, bone, liver, and spleen Grossly, angiosarcomas tend to be highly hemorrhagic and deeply invasive.[4] Microscopically areas of angiosarcoma are represented by the freely anastomosing vascular channels lined by atypical endothelial cells, Clusters of reactive lymphocytes and clumps of hemosiderin are common.[4](Fig, 7a) (Fig. 7b).
 |
Click here to view |
Fig. 1: Chronic Siladenitis: Microscopically there is atrophic seromucinous salivary glands acini with duct surrounded by lymphocytic infiltrate. (H & E, 400X)
 |
Click here to view |
Fig. 2: Chronic sclerosing sialadenitis: microscopically there is acini of salivary gland with inter mixed duct of gland showing areas of fibrosis and congestion, lymphoplasmocytic infiltrate and lymphoid follicle formation.(H & E, 400X
Pleomorphic Adenoma
 |
Click here to view |
Fig. 3: (3a, 3b)- Microscopically epithelial and myoepithelial cells with condromyxoid stroma.Epithelial cells form glands, while myoepithelial show condroid myxoid stroma.(H & E, 400X).
Warthin tumor
 |
Click here to view |
Fig. 4: (4a, 4b)- Microscopically lymphoid tissue is prominent with germinal canters. Lymphoid tissue covered with large epithelial cells. (H & E 100X). This cells arranged in 2 layer. The laminar cells are more tall columnar and outer discontinuous layer of small cells at base. Stroma beneath contains lymphocytic infiltrate. (H & E 400X).
Nerve sheath myxoma
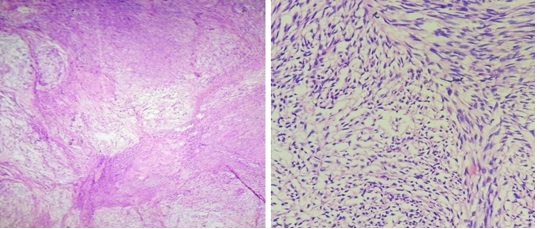 |
Click here to view |
Fig. 5: (4a, 5b)- Microscopically prominent multinodularity with fibrous border and presence of epithelial like cells.(H & E 100X).Epithelial cells and distinct fascicular or plexiform arrangement of cells.(H & 400X).
Mucoepidermoid Carcinoma
 |
Click here to view |
Fig. 6: (6a,6b)- Microscopically multicystic areas lined by mucin secreting cells, intermediate and well differentiated squamous cells (H & E 100X). Few of cysts are filled with mucus material. Peripheral areas show presence of salivary gland tissues with chronic inflammatory infiltrate.(H & E 400X).
Poorly differenciated angiosarcoma
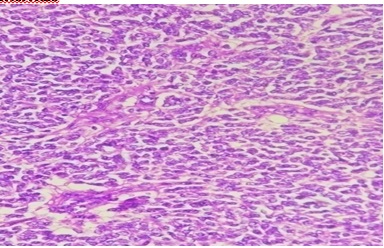 |
Click here to view |
Fig. 7: Microscopically sheets of tumor cells with ovoid nuclei and moderate amount of pale eosinophilic cytoplasm, focal attempt of RBC filled vascular and sinusoidal space formation secondary extravasations of RBC present.Tumor necrosis, tumor giant cells and atypical mitosis present. Mitotic count is 5-6/10 HPF.(H & E 400X).
The Present study is a retrospective study of lesions of salivary glands carried out in the Department of Pathology, GMERS Medical College,SOLA, over a period of 5 years.
The approach was to study the various histopathological types of salivary gland lesions, their classification and thorough study of lesions of salivary glands and to compare the observed findings to similar studies in relation to incidence, age, sex and risk factor distribution
Following observations are noted.
During the specified period, total of 66 cases of salivary gland lesions were studied.
Mean age observed was 39.5 years with an age range of 3 to 72 years.
There were 51 males (77.27%) and 15 females (22.72%) with a M:F ratio of 3.4:1
Parotid was the most common site of lesion 45 (68%).
Maximum cases were neoplasms - 44 cases (67%) and the non-neoplastic lesions were 22 cases (33%)
Among the neoplasms, 42 cases were benign (95%), and 02 cases were malignant (05%).
The majority of cases among non-neoplastic lesions were inflammatory lesions and sialadenitis
Majority of cases among benign salivary gland tumors were pleomorphic adenoma. The mucoepidermoid carcinoma was the only recognized malignant tumor followed by undifferentiated malignant tumor.
Conflicts of Interest: None.
How to cite : Kapuriya D, Pandya H, Bhalodia J, Histopathological study of non-neoplastic and neoplastic lesions of salivary gland. IP Arch Cytol Histopathol Res 2019;4(1):75-81
This is an Open Access (OA) journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.