
Print ISSN: 2581-5725
Online ISSN: 2456-9267
CODEN : IACHCL
IP Archives of Cytology and Histopathology Research (ACHR) open access, peer-reviewed quarterly journal publishing since 2016 and is published under the Khyati Education and Research Foundation (KERF), is registered as a non-profit society (under the society registration act, 1860), Government of India with the vision of various accredited vocational courses in healthcare, education, paramedical, yoga, publication, teaching and research activity, with the aim of faster and better dissemination of knowledge, we will be publishing the article more...Null
Author Details :
Volume : 4, Issue : 1, Year : 2019
Article Page : 82-86
https://doi.org/10.18231/2456-9267.2019.0014
Abstract
Introduction: Lymphadenopathy is seen commonly in patients attending the medical outpatient departments. FNAC is an easy and rapid diagnostic test. FNAC gives early direction to treatment protocol to be followed.
Aim: To study the different cytological spectrum associated with various lymphadenopathy and different lesions with respect to age and sex.
Materials and Methods: In our study, all cases of peripheral lymphadenopathies who had come to the cytology department for FNAC over a period of 3 years from 1st July 2015 to 1st July 2018 were included. It was a retrospective study.
Results: During a course of threeyears a total of 100 cases were received and were studied. Of these 6 cases were inconclusive due to unsatisfactory and haemorragicsmears; 83 cases were benign and 11 cases were neoplastic. The ages of patients were from 6 months to 65 years. Males were 54 and females were 46 in number. Reactive (27 cases), granulomatous (30 cases), Tuberculosis (4 cases), suppurative (14 cases), necrotic (5 cases), lymph node with filariasis (2 cases), metastasis (8 cases), lymphomas (3 cases).
Conclusion: FNAC is an easy, quick and good test to offer rapid diagnosis for lymphadenopathies and guide towards appropriate and timely treatment without the need of biopsy.
Keywords: FNAC, Lymphadenopathy, Benign, Neoplastic, Reactive, Granulomatous, Metastasis.
Lymphadenopathy is seen commonly in patients attending the medical outpatient deparments.[1] The spectrum of diseases varies from an inflammatory process to a neoplastic lesion.[2]
FNAC is an easy, quick and appropriate test for diagnosing lymphadenopathy.[3]The knowledge of the spectrum of lymphadenopathy in a given geographical region is important for making a definitive diagnosis. Tuberculosis is a common cause of lymphadenopathy and should be considered in every case of granulomatous lymphadenopathy unless proved otherwise.[4]
FNAC has pivotal role in the evaluation of peripheral lymphadenopathy and it can be used as an alternative to excision biopsy.[4]
The retrospective study was done at pathology department, TSM medical college Lucknow over a period of 3 years from 1stjuly 2015 to 1stjuly 2018. A total of 100 cases of peripheral lymphadenopathy those that were palpable on examination were included, non-palpable were excluded.
In each instance a brief history and physical examination along with evaluation of relevant investiation if available, was carried out. The FNAC procedure was performed by a cytopathologist using a needle attached to 10ml syringe. The aspirated material was immediately smeared onto slides. Few slides were immediately immersed in 95% ethanol and remaining air dried.
The air dried smears were routinely stained by Giemsa stain & alcohol fixed smears stained by PAP method. Special stains like Ziehl-Neelson for AFB were done whenever required.
All the stained smears were evaluated by cytopathologist. Diagnosis was based on cytological features and clinico-cytological correlation. At the end of the study data were analysed.
Results
Out of 100 patients with peripheral lymphadenopathy, the ages of patients were from 6 months to 65 year in which 54% were males and 46% were females. Sex distribution is shown in the Table 1
Table 1: Sex distribution of different lymph node lesions
|
Sex |
Granulomatous |
Reactive |
Suppurative |
Mets |
Necrotic |
TB |
HL cannot be ruled out |
NHL |
Filaria |
Inconclusive |
Total |
|
Male |
17 |
14 |
6 |
7 |
1 |
3 |
1 |
0 |
2 |
2 |
53 |
|
Female |
13 |
13 |
8 |
1 |
4 |
1 |
2 |
1 |
0 |
4 |
47 |
Six cases were inconclusive. 83 cases were inflammatory and 11 cases were neoplastic
Table 2 shows the cytological diagnosis of 100 patients with lymphadenopathy.
Among the non-neoplastic lymph node lesions, granulomatous lymphadenitis (30 cases) was the most common followed by reactive lymphadenopathy (27 cases), Suppurative –necrotic lesions (19 cases), micro filarial lymphadenitis (2 cases), tuberculosis (4 cases).Among the neoplastic lymph node lesions commonest was metastasis (8 cases), lymphoma (3 cases)
Table 2: Distribution of FNAC diagnosis of 100 cases of lymphadenopathy
|
Cytological diagnosis |
Number of cases |
Percentages% |
|
Granulomatous lymphadenitis |
30 |
30 |
|
Reactive lymphadenitis |
27 |
27 |
|
Suppurative lymphadenitis |
14 |
14 |
|
Metastatic lymphadenitis |
08 |
08 |
|
Necrotic lymphadenitis |
05 |
05 |
|
Tubercular lymphadenitis |
04 |
04 |
|
Hodgkin’s lymphoma cannot be ruled out |
03 |
03 |
|
NHL |
01 |
01 |
|
Micro filarial lymphadenitis |
02 |
02 |
|
Inconclusive |
06 |
06 |
|
Total |
100 |
100 |
It has been noted that cervical lymph nodes were involved most commonly (84%) followed by axillary (3%), inguinal (2%) and generalized (1%) as shown in the Table 3
Table 3: Distribution of lymph node groups involved
|
Lymph node group involved |
Total number of cases |
|
Cervical |
84 |
|
Axillary |
7 |
|
Supraclavicular |
2 |
|
Inguinal |
4 |
|
Generalised |
1 |
|
Forearm/arm |
2 |
The ages of patients were from 6 months to 76 years. The youngest patient with lymphadenopathy was diagnosed as Suppurative lymphadenitis and the oldest patient was diagnosed with metastatic adenocarcinoma. Metastatic deposits were more common in the extremes of ages. Tuberculosis and granulomatous pathology were more common in the 10-40years.The age distribution of patients with lymphadenopathy are shown in Table 4
Table 4: Age distribution of lymph node lesions
|
Ages In years |
Granulomatous |
Reactive |
Suppur |
Mets |
Necrotic |
TB |
HL cannot be ruled out |
NHL |
Microfilaria |
Inconclusive |
Total |
|
0-10 |
2 |
9 |
3 |
0 |
0 |
1 |
0 |
0 |
0 |
1 |
16 |
|
11-20 |
13 |
11 |
6 |
0 |
1 |
0 |
0 |
0 |
0 |
1 |
32 |
|
21-30 |
5 |
3 |
1 |
0 |
1 |
1 |
2 |
0 |
0 |
2 |
15 |
|
31-40 |
7 |
1 |
1 |
0 |
0 |
2 |
0 |
0 |
0 |
0 |
11 |
|
41-50 |
2 |
3 |
2 |
2 |
2 |
0 |
0 |
0 |
1 |
0 |
12 |
|
51-60 |
1 |
0 |
0 |
2 |
1 |
0 |
1 |
1 |
1 |
2 |
09 |
|
>61 |
0 |
0 |
1 |
4 |
0 |
0 |
0 |
0 |
0 |
0 |
05 |
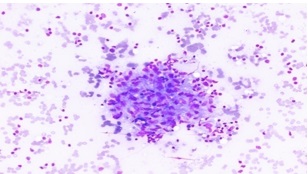
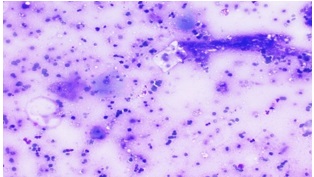
Granulomatous lymphadenitis was diagnosed by the presence of epithelioid cell granulomas as shown in Fig1 as Granulomatous Lymphadenitis in Giemsa stained smear at 400X magnification. Ziehl Neelson stain was negative for AFB. This formed the predominant pathology. Reactive lymph node hyperplasia was diagnosed by the presence of a polymorphous population of lymphoid cells composed of centrocytes, centroblasts, small lymphocytes and immunoblasts along with tingible body macrophages. Suppurative lymphadenitis was diagnosed by the presence of sheets of neutropils.Necrotic lymphadenitis was marked by extensive areas of necrosis. Ziehl Neelson stain was negative for AFB.
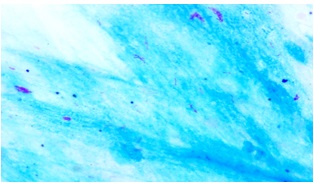
Tuberculosis was diagnosed when AFB was positive in Zeil Neelson stain as shown in fig. 2 as Acid Fast Bacilli Positive bacilli in lymph node aspirate in ZN stain in oil magnification (1000x)
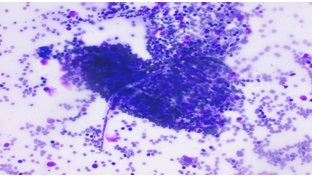
Microfilaria was noted in lymph node aspirate as shown in fig. 3 (microfilaria in lymph node aspirate in Giemsa stained smear at magnification of 400x)
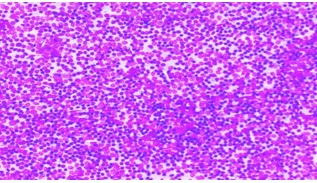
Non-Hogkins lymphoma was diagnosed by the presence of a monomorphic population of lymphocytes scattered singly in a highly cellular smear and the absence of RS cell as shown in Fig. 4 (Non Hodgkin’s lymphoma on FNAC lymph node on Giemsa stained smear at magnification of 200x)
Hodgkins lymphoma cannot be ruled out was diagnosed based on presence of granulomas and R-S like cells scattered in a reactive background. So biopsy was advised for further confirmation.
Metastatic deposits were diagnosed based upon cytological patterns and cellular details. Majority were from Squamous cell carcinoma as shown in fig. 5 depicting squamous cell carcinoma metastasis in lymph node aspirate on Giemsa stain at magnification 200x followed by adenocarcinoma as shown in the following Table 5
Table 5: Different metastatic deposits in lymph nodes
|
Metastatic lesions |
Males |
Females |
Total |
|
Squamous cell ca |
5 |
0 |
5 |
|
Adenocarcinoma |
1 |
1 |
2 |
|
Undifferentiated |
1 |
0 |
1 |
Table 6: Comparison of current study with other studies evaluating the causes for lymphadenopathy
|
Author |
Total cases |
Reactive |
Granulomatous
|
Suppurative/ necrotic |
Lymphoma |
Tuberculosis |
Metastasis |
Inconclusive |
Others (nonspecific) |
|
Current study 2019 |
100 |
27 |
30 |
19 |
04 |
04 |
08 |
06 |
2(microfilaria) |
|
Badge S A et al 2018 |
310 |
25 |
109 |
5 |
3 |
151 |
12 |
5 |
- |
|
Sheela KM et al 2017 |
122 |
29 |
- |
1 |
29 |
41 |
20 |
- |
1 |
|
Gayatri MN et al 2015 |
1774 |
465 |
262 |
70 |
13 |
260 |
376 |
- |
328 |
|
Attalla M et al 2014 |
235 |
108 |
110 |
- |
10 |
- |
05 |
- |
02 |
 |
Click here to view |
Fig. 1: Granulomatous Lymphadenitis
 |
Click here to view |
Fig. 2: Acid Fast Bacilli Positive in ZN Stain of lymph node aspirate
 |
Click here to view |
Fig 3: Microfilaria in lymph node aspirate
 |
Click here to view |
Fig. 4: Non Hodgkins lymphoma on FNAC lymph node
 |
Click here to view |
Fig. 5: Squamous cell carcinoma metastasis in lymph node
Lymphadenopathy is a commonly seen clinical condition requiring quick and accurate diagnosis so that a proper treatment regimen can be started at the earliest. FNAC is a completely safe, quick and appropriate method for early diagnosis of lymphadenopathy reducing the need of excision biopsy.[1]
In the present study 100 cases of palpable peripheral lympadenopathyfor a period of three years were studied retrospectively.
Aspirates were inconclusive in six cases due to unsatisfactory smears. The causes for unsatisfactory smears were scanty cellularityor hemorrhagic smears. Aspirates were benign in 83% and metastatic deposits were found in 8% and lymphoma in 3%. The pattern of lesion varied from nonneoplastic lesion like granulomatous, reactive
suppurative, necrotic, tubercular, microfilarial to neoplastic lesions like metastatic lymphadenopathy and lymphomas.
In our study cervical lymph nodes were involved mostly (84%) followed by axillary lymph nodes (7%). In a study done by Gayathri etal cervical group was the most commonly involved(74.6%) followed by axillary lymph nodes.?1;Comparison of current study with other studies evaluating the causes for lymphadenopathy is depicted in the table 6.
In a study done by PanditAA et al male to female ratio was equal our study was almost similar with slight male predominance. (M:F::1.1:1).?2;
In Granulomatous pathology was the most common cause of lymphadenopathy in our study similar to study done by Mir Attaullahetal.?3;
Study done by Badge et al showed 32% cases of granulomatous lymphadenitis. The granulomatous cases showed the presence of granulomas composed of epithelioid cells, histiocytes and lymphocytes but were negative for Acid fast bacilli on ZN stain. And those positive for AFB were diagnosed as tuberculosis.[4]In our study maximum cases were reported as granulomatous. (30%) based on similar cytological features. while suppurative cases showed only sheets of neutropils and no granulomas.[4]
.In our study squamous cell carcinoma was the most common metastatic malignancy followed by adenocarcinoma similar to a study done by PramodPathyetal in which squamous cell carcinoma was the most common metastatic malignancy followed by adenocarcinoma and poorly differentiated carcinoma.[5]
In a study done by Dr. Ripunjaya Mohanty et al cervical group was the most common to be involved by metastasis with squamous cell carcinoma being the most common histological type [6]
In our study majority of patients with metastatic squamous cell carcinoma in lymph nodes were above 50years. The finding of the study supported that metastatic squamous cell carcinoma is frequent after age of 40 years.[7]
Lymphoproliferative disorders were diagnosed in only 4 cases and formed a very small percentage of the total pathologies reported which correlated with study done by Ramanan D et al in 2016 who also reported 4% cases.[8]
In a study done by Akanksha Misra et al in 2017 Non-Hodkins lymphoma was diagnosed in 2.5 % cases.[9] while in our study Non-Hodkins lymphoma was diagnosed in only 1% cases.
Tuberculosis is the commonest cause of lymphadenopathy in developing countries and should be considered in every case of granulomatous lympadenopathy unless proved otherwise.[10]In their study, Khajuria et al found tuberculosis as the most common diagnosis.?1;° while in our study TB cases formed only 4% cases based on AFB stain positivity on Zeihl Neelsons staining.
The most commonly affected lymph nodes were cervical followed by supraclavicular, axillary, inguinal and post auricular in a study done by Sheela M et al in 2017.[11]In our study also cervical was the commonest group involved.
In our study the highest number of cases were seen in 11-20years while in another study by Silas et al highest number of cases were in ages 10-14 years.[12]and in another study by Mishra et al most common etiology of affected lymph nodes was tuberculous lympadenitis.[13]
In a study done in 2014 by Bhavani et al, the most common causes of cervical lympadenopathy were tuberculosis, reactive hyperplasia and metastatic malignancies particularly squamous cell carcinoma.[14] while in a study done by Devi Thaker et al in 2017 reactive hyperplasias were the most commonly found lesion in lymphadenopathies.[15]In our study most common cause was granulomatous followed by reactive and suppurative and then metastasis and lymphomas.
FNAC is an easy and rapid diagnostic test for diagnosing inflammatory as well as neoplastic lesions. It is safe and appropriate tool for providing definite diagnosis in lymph nodes aspirates where biopsies can be avoided. The knowledge of cytological patterns of various lesions of lymph nodes in an area helps in better approach to the diagnosis. FNAC is suitable for developing countries with financial constraints where it can minimize the economic burden and avoid the need for excision biopsy.
Conflicts of Interest: None.
How to cite : Sharma H B, Bansal M , Kumar N, Gupta M , Spectrum of lymphadenopathy on fine needle aspiration cytology-A 3 year retrospective study in a tertiary care centre. IP Arch Cytol Histopathol Res 2019;4(1):82-86
This is an Open Access (OA) journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.