- Visibility 327 Views
- Downloads 56 Downloads
- Permissions
- DOI 10.18231/j.achr.2020.029
-
CrossMark
- Citation
A comparative study of conventional pap smear with liquid based cytology for early diagnosis of cervical cancer
- Author Details:
-
Kalathingal Kamarunisha Aboobacker, *
-
M H Shariff
Abstract
Introduction: Cervical cancer is the third most common female malignancies worldwide with high mortality. Since the introduction of conventional PAP smear (CPS) mortality from cervical cancer has reduced considerably. Evidence shows that alternative method liquid based cytology (LBC) is more sensitive and accurate for the detection of both squamous and glandular lesions of the cervix.
Objective: The main objective of this study is to compare conventional PAP smear and liquid based cytology and observe for morphologic features, sensitivity, specificity and positive predictive values.
Materials and Methods: This was a prospective study conducted on 240 cases and samples were processed for CPS and LBC. Cytobrush was used for LBC which was suspended and detached in the preservative fluid and processed by manual method. Histopathological correlation was done in 32 cases and HPV DNA testing was done in 76 cases.
Results: LBC showed higher specimen adequacy, cellularity, clean background and uniform distribution of cells than CPS. Overall sensitivity of LBC (83.33%) and negative predictive value was more in LBC (92.85%) as compared to CPS.
Conclusion: In this study LBC showed improved specimen adequacy, better cytomorphological features and higher detection of epithelial cell abnormality. Thus LBC has higher detection rate of precancerous lesion than CPS.
Introduction
Cervical cancer is found to be third most common malignancy affecting women worldwide. A devastating disease with an estimated 20 million cases by the year 2020.[1] More than 85% cases and 88% deaths from cervical cancer occur in developing countries, where women often lack access to cervical cancer screening and treatment. The magnitude of the problem of cancer in the Indian Sub-Continent is alarming[2] and accounts for one-fourth of the global cervical cancer burden.[3]
Cervical screening helps in early detection of cancer and thus reducing cancer deaths.[4] The primary screening test for cervical cancer the Papanicolaou (Pap) smear is responsible for diagnosing cancerous and precancerous lesions. It is a convenient, cost-effective, simple test and performing this test is considered as a health promotion behaviour.[5]
Pap test has high specificity of 98-99 % and sensitivity ranges from 50-75%. [6], [7] This led to drastic reduction in the incidence of cervical carcinoma. But the Pap test had a high false negative rate due to sampling errors, presence of blood or mucus (obscuring) material, screening errors and interpretation errors.
Liquid based cytology (LBC) is the most accepted method for detection of premalignant lesion and improves the smear sensitivity. The advantage of LBC include removal of blood and mucus, obscuring cells, reduction of unsatisfactory smears and provision of cells for detection of HPV, presence of residual sample for performing ancillary techniques such as immunocytochemistry. LBC gives standardized slides containing a monolayer of well stained well preserved cells which is easier to interpret than the conventional smears. So the aim of this study is to compare the results of conventional PAP smear(CPS) and liquid based preparation and to correlate the results with the histopathological findings.
Ethical clearance
The study protocol was approved and ethical clearance taken from the University ethics committee.
Materials and Methods
This prospective study was conducted on 240 patients selected randomly in the Department of Pathology from December 2016 to September 2018. In this study we had proposed to conduct a comparative analysis of cervical cytology based on result, predictive value by using conventional Pap smear with manual method based liquid based cytology. Women between the ages of 21 to 65 years, women presenting with white discharge per vaginum, post coital bleeding or irregular bleeding, unhealthy cervix on speculum examination and pain in abdomen were included in the study. Non co-operative patients, patients who do not give consent, women who had undergone hysterectomy with removal of cervix, patients with massive bleeding per vaginum, Pregnant women and treated cervical carcinoma cases were excluded from the study.
After obtaining proper consent, detailed history was taken and physical examination was done. Specimens were first obtained for Conventional PAP, Ayre’s spatula was inserted into the cervix and gently rotated at 360º. Sample was smeared onto a grease free slide, fixed in alcohol stained with rapid PAP stain.
For Liquid based cytology, manual LBC method was followed. The endocervical brush was inserted into the endocervical canal and rotated 360º 3-4 times. Brush was detached and placed into a vial containing fixative for transport composed of 10%formalin 50ml, sodium chloride 0.5gm, sodium citrate 0.5gm and isopropyl alcohol 50ml. The vial is then closed and shaken to obtain a homogenous mixing. The vial is taken to the lab where it is again shaken with the vortex to obtain a homogenous mixture. This mixture was centrifuged at 2000 rpm for 10 minutes. The supernatant was discarded. To the cell pellet at the base of the tube, 1.5 ml of polymer solution was added. This mixture was once again mixed with vortex and centrifuged. With the help of the micropipette 50 μl of the suspensions was taken and placed over the slide in a circular manner. The slides are dried and stained with conventional pap stain.
For histopathological examination
All specimen received in the department following surgery were kept for overnight fixation in 10% neutral buffered formalin. Grossing was performed according to College of American Pathologist (CAP) protocol. The tissue bits given were processed overnight using a Leica TP1020 Semi-Enclosed B enchtop Tissue Processor (Leica Biosystem, Wetzlar, Germany. The sections were stained with hematoxylin and Eosin on a Leica ST 5010 Autostainer XL(Leica Biosystems, Wetzlar, Germany).
HPV DNA
Wherever possible, ancillary techniques were applied and HPV DNA testing was done on the residual cytobrush sample. DNA was extracted from the cytobrush sample and conventional PCR was carried out for the detection of HPV common and HPV 18 E6 and E7 oncoproteins.
Statistical analysis
The data was entered into Microsoft Excel 2016 worksheets and then further statistical analysis was performed on IBM SPSS version 23.
Results
Most of the patients in this study were in fifth decade. Minimum number of cases (n=22, 9.2%), belonged to more than 60years age group and maximum number of cases (n=100, 41.7%) belonged to 40-49age group. Cases with 2 children were 40.4% and 3 children were 42.5% which also represented most number of cases with epithelial cell abnormality.
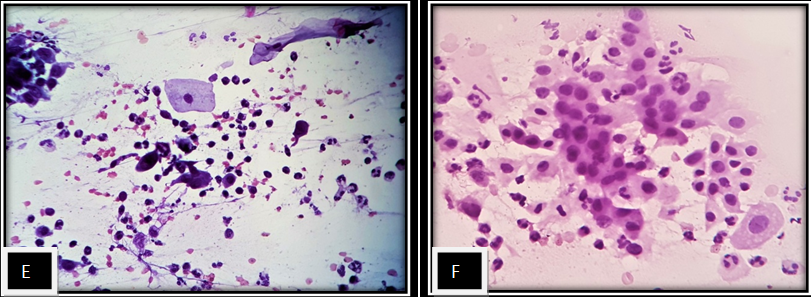
Women presented with complaints of white discharge per vaginum (19%), bleeding per vagina(15%), dysfunctional uterine bleeding(2.9%), pain in abdomen(4.6%), prolapse(6.7%), burning micturation (0.8%) or came for routine checkup (50.8%). LBC detected abnormality of 24cases(10%) and CPS detected abnormality of 22cases (9.1%). In CPS 92% cases were satisfactory while 95% cases were satisfactory in LBC.
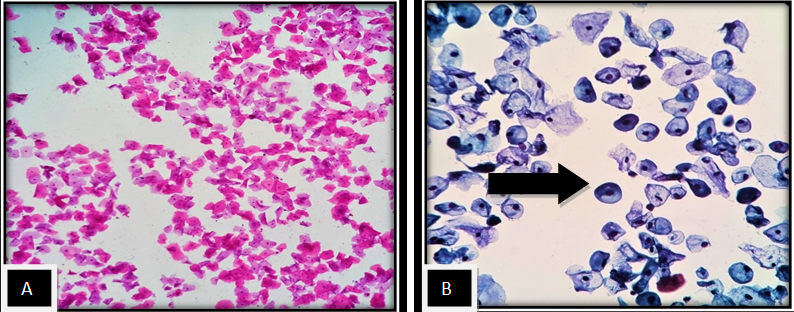
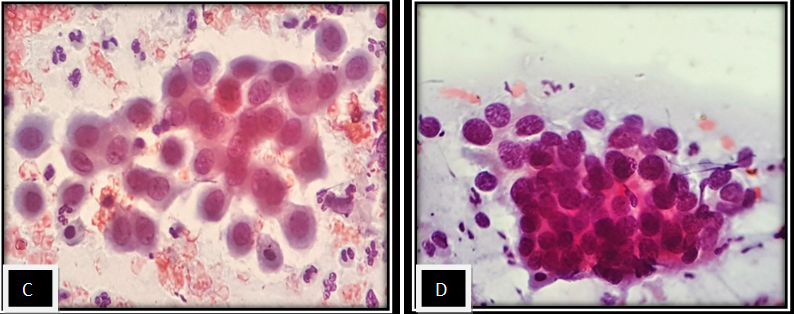
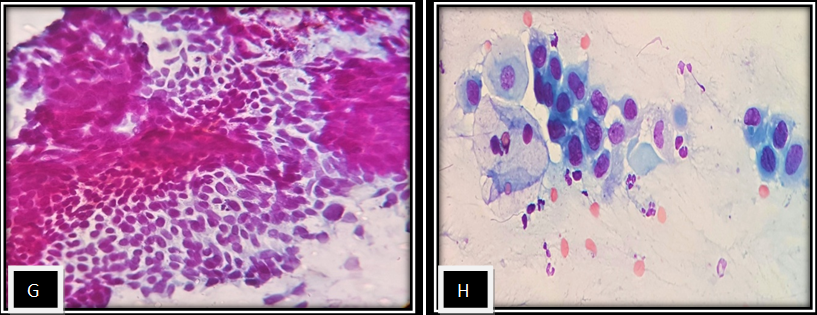
Cytomorphological features are compared between CPS and LBC in [Table 1]. Statistically significant Pvalue was seen in cellularity, uniform distribution of cells, clean background, artefact cellular overlapping and cellular change. Overall sensitivity of PAP was 71% and LBC 83.33% while specificity 93.33% and 87.5% respectively. Positive predictive value of PAP was 83.33% while it was 71.42% in LBC. Negative predictive value of PAP was 87.5% and LBC was 93.33%. The difference in interpretation of results by the two methods were statistically significant and is shown in [Table 2].
| Cytomorphological studies | PAP | LBC |
| Cellularity | 223(93%) | 231(96.25%) |
| Clean background | 10(4.2%) | 216(90%) |
| Uniform distribution | 14(5.8%) | 166(69.2%) |
| Cellular overlapping | 208(86%) | 80(33.3%) |
| Architectural change | 205(85.4%) | 30(12.5%) |
| Cellular change | 201(83.8%) | 35(14.6%) |
| Nuclear change | 33(13.8%) | 47(19.6%) |
| Inflammatory cells | 92.2% | 22.6% |
| Diagnosis | PAP | LBC | χ2 | DF | P-value |
| NILM | 103 (42.9%) | 135 (56.25%) | 2407.51 | 144 | <0.001 |
| Inflammatory smear | 59 (24.9%) | 35 (14.6%) | |||
| Atrophic smear | 19 (7.9%) | 18 (7.5%) | |||
| Bacterial vaginosis | 14 (5.8) | 14 (5.8%) | |||
| Candidiasis | 4 (1.7%) | 4 (1.7%) | |||
| ASCUS | 7 (2.9%) | 8 (3.33%) | |||
| ASC-H | 1 (0.4%) | 1 (0.4%) | |||
| HSIL | 6 (2.5%) | 5 (2.08%) | |||
| LSIL | 1 (0.4%) | 1 (0.4%) | |||
| SCC | 5 (2.1%) | 6 (2.5%) | |||
| Adenocarcinoma | 1 (0.4%) | 1 (0.4%) | |||
| AGC NOS | 1 (0.4%) | 1 (0.4%) | |||
| Unsatisfactory | 19 (7.9%) | 11 (4.6%) | |||
| Total | 240 | 240 |
[Table 3]shows histopathological examination findings in 32 cases. Out of the 12 cases of NILM cases in PAP 8 cases had chronic cervicitis and 1 case was of serous borderline carcinoma ovary in HPE. Similarly comparison between HPE and LBC showed out of 18 cases of NILM in PAP, 10 cases had chronic cervicitis, 2 case of prolapse, 2 case of papillary endocervicitis,1 case of necrotising granulomatous lesion and 1 case was of serous borderline carcinoma ovary in HPE.
| Diagnosis | HPE | Percentage |
| Chronic cervicitis | 16 | 50% |
| Prolapse | 2 | 6.25% |
| Endocervical polyp | 3 | 9.4% |
| Papillary endocervicitis | 2 | 6.25% |
| Necrotising granulomatous inflammation | 1 | 3.1% |
| Carcinoma | 8 | 25% |
| Total | 32 | 100 |
| Total sample | PCR positive samples | PCR negative samples | Positive predictive value | Negative predictive value |
| Cytological positive cytobrush samples (n=6) | 02 | 04 | 33.4% | 88.6% |
| Cytological negative cytobrush samples (n=70) | 08 | 62 |
[Table 4] shows Comparison of cytological findings and HPV DNA molecular findings of cytobrush samples done in 76 cases along with positive and negative predictive value. Out of which 10 cases were PCR positive. 6 cases of cytological positive samples were cases of HSIL, ASCUS and 70 cases were cytological negative samples which included NILM, inflammatory smear, bacterial vaginosis and atrophic smear. Out of 6 cytological positive cases 2 were PCR positive and 4 were PCR negative. Whereas out of 70 cytological negative cases 8 cases were PCR positive and 62 cases were PCR negative.
Discussion
Widespread cervical screening has reduced the incidence of cervical cancer by more than 50%.[8] Clarity of microscopic features, small area to be screened, decreased unsatisfactory results, improved sample processing along with the potential for performing additional tests HPV DNA testing makes LBC more promising and acceptable among gynecologist, colposcopists and pathologists.
Out of 240 cases analysed, age of presentation in most cases (41.7%) were seen in the fifth decade of life similar to Chinaka C et al [9] (31.33%) and Taylor S et al [10] which also showed maximum number of cases in 40-49 age group. Parity 3 showed maximum number of cases (42.5%) in the present study similar to Khamankar S et al [11] (36.7%) while Budak M et al[12] & Macharia H C et al [13] showed most cases with parity 2. WDPV as a presenting complaint was also seen in studies done by Khamankar S et al, [13] Sharma J et al, [14] Sherwani RK et al[15] and Singh A et al.[16]
This study showed more satisfactory smears in LBC( 95% ) than in CPS (92%) similar to Hegde V et al [17] (PAP34% LBC67%), Sherwani R K et al [15] (PAP31.9% LBC83.1%), Chinnaka C et al [9] (PAP53.3% LBC83.3%), Dhananjaya C [18] (PAP84% LBC86%), Singh A et al [16] (PAP78.8% LBC92.5%) & Sharma J et al [14] (PAP92% LBC93%). Contrary to this finding, studies by Longatto-Filho A et al [19] (PAP34% LBC66%) and Ilter E et al [20] (PAP34% LBC66%) showed more satisfactory smears in PAP compared to LBC. The present study showed clean background, uniform distribution of cell more in LBC as compared to CPS similar to Hegde V et al,17 Dhanajaya C et al [18] and Nandini N M et al [21] According to Uttagawa M L et al [22] LBC presented clear background in relation to CPS.
Cellular overlapping, architectural change and cellular morphological change in our study was more in CPS than LBC similar to Kavatkar et al, [23] Nandini N M et al [21] and Hegde et al. [17] Strander et al [24] and Kirschner B et al [25] also showed more number of unsatisfactory smears in CPS than LBC. Cases diagnosed with NILM were more in LBC (55.4%) as compared to CPS (42.9%) in this study similar to Singh V B et al, [26] Singh U et al [27] and Dhananjaya C et al. [18] However studies done by Stabile S et al [28] and Beerman H et al [29] reported more number of NILM cases in CPS as compared to LBC. LSIL cases were equal in PAP and LBC in the present study and study done by Sherwani et al. [15] While studies done by Budak et al, [12] Beerman et al, [29] Stabile S et al, [28] Strander et al, [24] Longatto-Filho A et al [19] and Singh U et al [27] observed more cases of LSIL in LBC as compared to CPS.
The number of cases diagnosed with HSIL was more in LBC as compared to CS in studies conducted by Almonte M et al, [30] Chinaka C et al, [9] Sherwani R K et al, [15] Beerman H et al, [29] Uttagawa M et al [22] and Singh A et al [16] which was in concordance with the present study. Studies done by Stabile S et al [28] and Uttagawa M et al [22] which showed more cases diagnosed with ASCUS in LBC than in CS similar to the present study.
Studies conducted by Budak M et al [12] and Qureshi S et al [31] reported more cases of SCC in LBC than in CPS. Studies done by Budak M et al [12] and Stabile S et al [28] reported more cases of AGS-NOS in LBC as compared to CPS. Singh A et al, [17] Singh V B et al [26] and present study reported same number of adenocarcinoma cases in CPS and LBC .
LBC showed better performance and diagnostic accuracy than CPS. Similarly according to study conducted by Sykes P H et al[32], [30] 11 women diagnosed as micro invasive carcinoma was cytologically diagnosed as ASC-H and 9 case of histologically diagnosed and confirmed as ACIS were CIN2/3. Study conducted by Singh U et al [28] also showed better diagnostic accuracy for LBC (97.6%) as compared to CPS (79.16 %) with respect to HPE diagnosis. Similarly study by Stabile S A et al [28] found that LBC had better concurrence to diagnose atypical cells and the cyto histological concordance was more in LBC than in CPS.
Conclusion
CPS is a simple cost effective tool for cervical screening. Manual LBC overcomes the high false positive and false negative results of CPS and also can be further used for ancillary testing such as HPV DNA testing. In this study LBC by manual method showed improved specimen adequacy, better cytomorphological features and better detection of epithelial cell abnormality. The advantage of LBC over CPS was observed in reducing unsatisfactory smears for evaluation and increasing the sensitivity and negative predictive value of the test. The manual LBC has an edge over the automated LBC Thinprep and Surepath methods in cost effectiveness.
Disclosure
This study was done as part of thesis from Yenepoya Medical college, Mangalore, 575018 Karnataka
Source of Funding
None.
Conflict of Interest
None.
References
- Kurman RJ, Carcangiu ML, Herrington CS, Young R. WHO Classification of Tumours of Female Reproductive Organs. . 2014. [Google Scholar]
- Rao DN, Ganesh B. Estimate of cancer incidence in India in 1991. Indian J Cancer. 1998;35(1):10-18. [Google Scholar]
- Nath J, Bhattacharyya A, Deka H. Comparative study between pap smear and visual inspection with acetic acid (via) in screening of CIN and early cervical cancer. J Midlife Health. 2015;6(2):53-8. [Google Scholar]
- Senapathy JG, Umadevi P, Kannika PS. The Present Scenario of Cervical Cancer Control and HPV Epidemiology in India: an Outline. Asian Pacific J Cancer. 2011;12:1107-15. [Google Scholar]
- Keshavarz Z, Simbar M, Ramezankhani A. Factors for performing breast and cervix cancer screening by Iranian female workers: a qualitative-model study. Asian Pac J Cancer Prev. 2011;12(6):1517-22. [Google Scholar]
- Fahey MT, Irwig L, Macaskill P. Meta-analysis of Pap Test Accuracy. Am J Epidemiol . 1995;141(7):680-9. [Google Scholar]
- Nanda K, McCrory DC, Myers ER, Bastian LA, Hasselblad V, Hickey JD. Accuracy of the Papanicolaou Test in Screening for and Follow-up of Cervical Cytologic Abnormalities. Ann Intern Med. 2000;132(10):810-9. [Google Scholar]
- Vaghela BK, Vaghela VK, Santwani PM. Analysis of abnormal cervical cytology in Papanicolaou smears at tertiary care center - A retrospective study. IJBAR. 2014;05(01):47-49. [Google Scholar]
- Chinaka CC, Abudullahi M, Mohammed OM. A Comparative Study on the Use of Liquid Based Cytology and Conventional Pap Smear in Cervical Screening. JMMR. 2014;2(4):40-50. [Google Scholar]
- Taylor S, Kuhn L, Dupree W, Denny L, Souza MD, Wright TC. Direct comparison of liquid-based and conventional cytology in a South African screening trial. Int J Cancer. 2006;118(4):957-62. [Google Scholar]
- Khamankar ST, Belekar V, Bhagat V, Baviskar SR. Cervical cancer screening: risk factors for cervical neoplasia among rural women of Nanded Maharashtra. IJMHS. 2014;4:312-6. [Google Scholar]
- MB, Senturk M, Kaya C, Akgol S, Bademkiran M, Ali E. A Comparative Study of Conventional and Liquid-Based Cervical Cytology. Ginekol Pol . 2016;87:190-3. [Google Scholar]
- CM, JC, EB, LM. A comparative analysis of conventional Pap smear cytology, liquid based cytology and colposcopy clinical impression with colposcopy biopsy histology as gold standard in women undergoing colposcopy in Kenyatta National Hospital. Int J Reprod Contracept Obstet Gynecol. 2014;3(1):58-63. [Google Scholar]
- Sharma J, Toi PC, Siddaraju N, Sundareshan M. Habeebullah SA comparative analysis of conventional and Surepath liquid-based cervicovaginal cytology: a study of 140 cases. J Cytol. 2016;33(2):80-4. [Google Scholar]
- Sherwani R, Khan T, Akhtar K, Zeba A, Siddiqui F, Rahman K. ConventionalPap smearand liquid based cytology for cervical cancer screening - a comparative study. J Cytol. 2007;24(4):167-72. [Google Scholar]
- Singh A, Joshi C, Kujur P, Chandrakar K, Shrivastava S. Liquid-based cytology versus conventional cytology for evaluation of cervical cytology in a tertiary care center of Chattisgarh. Int J Scientific Study. 2016;4(9):161-7. [Google Scholar]
- Hegde V, Nambiar S, Yadav N. Efficacy of centrifuged liquid-based cytology over conventional cytology: A comparative study. J Can Res Ther. 2017;13:951-5. [Google Scholar]
- Dhananjaya C, Kumari MK. Comparison of Manual Liquid Based Cytology and Conventional Pap Smear in Cervical Cancer Screening. National J Lab Med. 2017;6(2):32-7. [Google Scholar]
- Longatto-Filho A, Levi JE, Martins TR, Cohen D, Cury L, Villa LL. Critical Analyses of the Introduction of Liquid-Based Cytology in a Public Health Service of the State of São Paulo, Brazil. Acta Cytol. 2015;59(3):273-7. [Google Scholar]
- İlter E, Midi A, Haliloğlu B, Çelik A, Yener A, Ulu �. Comparison of conventional and liquid-based cytology: do the diagnostic benefits outweigh the financial aspect?. Turk J Med Sci. 2012;42(1):1200-6. [Google Scholar]
- Nandini N, Nandish S, Pallavi P, Akshatha S, Chandrashekhar A, Anjali S. Manual Liquid Based Cytology in Primary Screening for Cervical Cancer - a Cost Effective Preposition for Scarce Resource Settings. Asian Pacific J Cancer Prev. 2012;13(8):3645-51. [Google Scholar]
- Utagawa M, Pereira SM, Makabe S, Maeda MY, Marques J, Santoro C. Pap Test in a High-Risk Population Comparison of Conventional and Liquid-Base Cytology. Diagn Cytopathol. 2004;31(3):169-72. [Google Scholar]
- Kavatkar A, Nagwanshi C, Dabak S. Study of a manual method of liquid-based cervical cytology. Indian J Pathol Microbiol . 2008;51(2):190-4. [Google Scholar]
- Strander B, Andersson-Ellström A, Milsom I, Rådberg T, Ryd W. Liquid-based cytology versus conventional Papanicolaou smear in an organized screening program. Cancer. 2007;111(5):285-91. [Google Scholar]
- Kirschner B, Simonsen K, Junge J. Comparison of conventional Papanicolaou smear and SurePathR liquid-based cytology in the Copenhagen population screening programme for cervical cancer. Cytopathol. 2006;17(4):187-94. [Google Scholar]
- Singh VB, Gupta N, Nijhawan R, Srinivasan R, Suri V, Rajwanshi A. Liquid-based cytology versus convetional cytology for evaluation of cervical Pap smears. Indian J Pathol Microbiol. 2015;58(1):17-21. [Google Scholar]
- Qureshi S, Singh U, Anjum, Negi N, Singh N, Goel M, et al. Comparative study between liquid-based cytology & conventional Pap smear for cytological follow up of treated patients of cancer cervix. Indian J Med Res . 2018;147(3):263-7. [Google Scholar]
- Stabile SAB, Evangelista DHR, Talamonte VH, Lippi UG, Lopes RGC. Comparative study of the results from conventional cervico-vaginal oncotic cytology and liquid-based cytology. Einstein (São Paulo). 2012;10(4):466-72. [Google Scholar]
- Beerman H, Dorst Ev, Kuenen-Boumeester V, Hogendoorn P. Superior performance of liquid-based versus conventional cytology in a population-based cervical cancer screening program. Gynecol Oncol. 2009;112(3):572-76. [Google Scholar]
- Almonte M, Ferreccio C, Winklerj, Cuzick J, Tsu V, Robles S. Takahashi7 and Peter SasieniCervical screening by visual inspection, HPV testing, liquid-based and conventional cytology in Amazonian Peru. Int J Cancer. 2007;121:796-802. [Google Scholar]
- Singh U, Singh N, Qureshi S, Foruin S, Negi N, Agarwal G. Liquid-based Cytology vs Conventional Cytology as a Screening Tool for Cervical Cancer in Postmenopausal Women. J South Asian Federation Obstet Gynaecol. 2017;9(2):159-63. [Google Scholar]
- Sykes P, Harker D, Miller A, Whitehead M, Neal H, Wells J. A randomised comparison of SurePath liquid-based cytology and conventional smear cytology in a colposcopy clinic setting. BJOG. 2008;115(11):1375-81. [Google Scholar]
How to Cite This Article
Vancouver
Aboobacker KK, Shariff MH. A comparative study of conventional pap smear with liquid based cytology for early diagnosis of cervical cancer [Internet]. IP Arch Cytol Histopathol Res. 2020 [cited 2025 Oct 22];5(2):141-146. Available from: https://doi.org/10.18231/j.achr.2020.029
APA
Aboobacker, K. K., Shariff, M. H. (2020). A comparative study of conventional pap smear with liquid based cytology for early diagnosis of cervical cancer. IP Arch Cytol Histopathol Res, 5(2), 141-146. https://doi.org/10.18231/j.achr.2020.029
MLA
Aboobacker, Kalathingal Kamarunisha, Shariff, M H. "A comparative study of conventional pap smear with liquid based cytology for early diagnosis of cervical cancer." IP Arch Cytol Histopathol Res, vol. 5, no. 2, 2020, pp. 141-146. https://doi.org/10.18231/j.achr.2020.029
Chicago
Aboobacker, K. K., Shariff, M. H.. "A comparative study of conventional pap smear with liquid based cytology for early diagnosis of cervical cancer." IP Arch Cytol Histopathol Res 5, no. 2 (2020): 141-146. https://doi.org/10.18231/j.achr.2020.029
