- Visibility 166 Views
- Downloads 30 Downloads
- Permissions
- DOI 10.18231/j.achr.2020.041
-
CrossMark
- Citation
Histoplasmosis of mesenteric lymphnode in an immunocompromised adult: FNAC diagnosis and its differentials
- Author Details:
-
Indranil Chakrabarti *
Abstract
Histoplasma capsulatum is an opportunistic fungus that is endemic in some countries and can cause severe widespread disease, particularly among the immunocompromised patients. A meticulous examination of aspiration smears in a proper clinical setting can provide a rapid and accurate diagnosis in lymphadenopathies caused by Histoplasma species.
Introduction
Histoplasmosis is an opportunistic fungal infection of worldwide distribution which is caused by the intracellular, thermally dimorphic fungus Histoplasma capsulatum.[1] The infection is acquired through respiratory route with the inhalation of spores of H. capsulatum which are present in soils contaminated by bird and bat excreta.[2] The clinical spectrum ranges from mild respiratory illness to more severe disseminated forms, which in turn, can have an acute, subacute or chronic presentation.[3] Disseminated Histoplasmosis is defined as Histoplasmosis affecting more than one site[1] and may affect lungs, lymph node, liver, spleen, bone marrow, adrenal gland, gastrointestinal tract as well as mucous membrane of the oral cavity.[2], [3], [4] In immunosuppressed individuals and extremes of age, they usually run a severe and progressive, often disseminated course.[2], [4] In India, which is non-endemic for Histoplasmosis, reported cases are sporadic.[1] Fine needle aspiration cytology can often clinch the diagnosis accurately with the added advantage of being a cheap, rapid and non-invasive procedure.
Case History
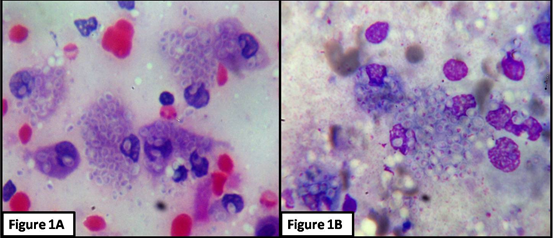
A 45-year old man presented to the outpatient department of Medicine with chronic diarrhea, weight loss and occasional abdominal pain for the last 2 months. He also complained of occasional low grade fever. On examination, the patient appeared emaciated and had mild pallor and icterus. There was mild hepatosplenomegaly but no peripheral lymphadenopathy. The Complete Blood Counts (CBC), Liver function tests (LFT), chest X-ray, stool examination and an abdominal ultrasound were done. The Hemoglobin was 9 gm/dl with normal WBC and platelet counts. The RBCs were mildly microcytic, hypochromic with mild anisopoikilocytosis. The stool examination was unremarkable other than positive occult blood test. The LFT showed a total bilirubin of 2.1 mg /dl with unconjugated bilirubin level of 1.8 mg/dl. The SGPT and SGOT levels were 80 U/L and 68 U/L respectively. The abdominal ultrasound revealed multiple mesenteric lymph nodes with the largest measuring 3X3 cm. The chest radiographs also showed multiple mediastinal lymph nodes. The patient was then advised for Mantoux test, image guided fine needle aspiration cytology (FNAC) of mesenteric as well as mediastinal lymph nodes and test for anti-HIV antibodies. An aspiration was done from the mesenteric lymph nodes by 22 G spinal needle and the aspirates were stained with Haematoxylin and Eosin (H&E) stain, Leishman-Giemsa(LG) stain and Ziehl Neelsen (ZN) stain. The smears showed multiple enlarged histiocytes with ill-defined granulomas in a background of reactive lymphocytes and hemorrhage. The histiocytes were studded with uniform sized (approximately about 4-5µm diameter) yeast like organisms with peripheral halo suggestive of Histoplasma capsulatum. ([Figure 1]A,B). There were few extracellular forms as well. No caseation, granuloma or multinucleated giant cells were appreciated in the smears. No AFB was found in the ZN stained slide. An unstained slide was stained with PAS stain which also highlighted the fungus. The Mantoux test was non-contributory but the patient turned out to be seropositive for HIV. A diagnosis of Histoplasmosis in a HIV positive patient was rendered, which were not aspirated. The clinical team was alerted and a possibility of disseminated Histoplasmosis was considered. An FNAC of mediastinal lymph node and bone marrow examination were planned and a treatment blueprint was formulated which comprised of the highly active antiretroviral therapy (HAART) and amphotericin B followed by Itraconazole. However, the patient unfortunately did not turn up even for collecting his reports of the FNAC.
Discussion
The present case highlights the use of diagnosis of Histoplamosis by aspiration cytology. FNAC has emerged as the diagnostic modality of choice in almost any pathological swelling. The nicely aspirated material in the hands of an experienced cytologist can be a real boon for the patient and the treating physician. The present case showed mostly intracellular forms of Histoplasma within the macrophages and showed characteristic morphology. The common differentials of the fungus include Cryptococcus neoformans, Leishmania donovani, Pneumocystis Jirovecii, Blastomyces dermatitidis , Coccidioides immitis and Toxoplasma gondii.
Cryptococci (size 4-12 µm) are similar in size, may have forms bigger than Histoplasma and usually show size variation. They show narrow neck budding and their capsule lights up in Mucicarmine and PAS stain while Histoplasma are not stained by mucicarmine. Leishmania amastigotes (size 2-4 µm ) also mimic Histoplasma but they have the characteristic kinetoplasts and being parasites, are not stained by PAS stain or Gomori Methenamine Silver (GMS) stain. Pneumocystis jirovecii have a frothy, proteinaceous “honeycomb”appearance and are located extracellularly with cysts being evident clearly in the GMS stained slides.
Blastomyces dermatitidis (size 8-15 µm) show thick walled spores with broad based budding and double-contoured cell walls which are PAS positive while Coccidioidomycosis immitis (size 10-80 µm) have spherules impregnated with endospores. Toxoplasma gondii are much smaller and rarely detected on aspirates. Aspirates may show, however, tissue cysts containing bradyzoites or intracellular tachyzoites. Thus after a careful comparison of size, location within or outside the cell, cytomorphology and special stains, a diagnosis of Histoplasmosis can be can be made with confidence on cytology smears.
Conclusion
To conclude, Histoplasmosis is an important differential of lymphadenopathies in a proper clinical setting even in non-endemic regions. The article also highlights that careful examination of cytology smears is accurate and rapid tool for diagnosis to the suspecting and experienced eyes.
Source of Funding
None.
Conflict of Interest
None.
References
- RSE, Sharma M, Tomar V. Disseminated histoplasmosis in an immunocompetent haweli dweller: A diagnosis and follow-up by endoscopic ultrasound-guided fine-needle aspiration. J Cytol. 2015;32(2):142-4. [Google Scholar]
- Jaiswal S, Vij M, Chand G, Misra R, Pandey R. Diagnosis of adrenal histoplasmosis by fine needle aspiration cytology: an analysis based on five cases. Cytopathol. 2011;22(5):323-8. [Google Scholar]
- Gupta P, Bhardwaj M. Cytodiagnosis of disseminated histoplasmosis in an immunocompetent individual with molluscum contagiosum-like skin lesions and lymphadenopathy. J Cytol. 2016;33(3):163-5. [Google Scholar]
- Gupta N, Arora SK, Rajwanshi A, Nijhawan R, Srinivasan R. Histoplasmosis: cytodiagnosis and review of literature with special emphasis on differential diagnosis on cytomorphology. Cytopathol. 2009;21(4):240-4. [Google Scholar]
How to Cite This Article
Vancouver
Chakrabarti I. Histoplasmosis of mesenteric lymphnode in an immunocompromised adult: FNAC diagnosis and its differentials [Internet]. IP Arch Cytol Histopathol Res. 2020 [cited 2025 Oct 10];5(3):188-189. Available from: https://doi.org/10.18231/j.achr.2020.041
APA
Chakrabarti, I. (2020). Histoplasmosis of mesenteric lymphnode in an immunocompromised adult: FNAC diagnosis and its differentials. IP Arch Cytol Histopathol Res, 5(3), 188-189. https://doi.org/10.18231/j.achr.2020.041
MLA
Chakrabarti, Indranil. "Histoplasmosis of mesenteric lymphnode in an immunocompromised adult: FNAC diagnosis and its differentials." IP Arch Cytol Histopathol Res, vol. 5, no. 3, 2020, pp. 188-189. https://doi.org/10.18231/j.achr.2020.041
Chicago
Chakrabarti, I.. "Histoplasmosis of mesenteric lymphnode in an immunocompromised adult: FNAC diagnosis and its differentials." IP Arch Cytol Histopathol Res 5, no. 3 (2020): 188-189. https://doi.org/10.18231/j.achr.2020.041
