Introduction
Renal replacement lipomatosis (RRL) is a rare benign condition in which the renal parenchyma, renal sinus, peri-renal spaces and renal hilum are replaced by adipose tissue.1, 2, 3 It is seen in 70% of cases with renal tuberculosis, infarction and calculus diseases. 2, 3, 4 This can mimic and can be confused with fatty neoplasm of kidney. We reported a case of RRL in patient along with review of literature.
Case Report
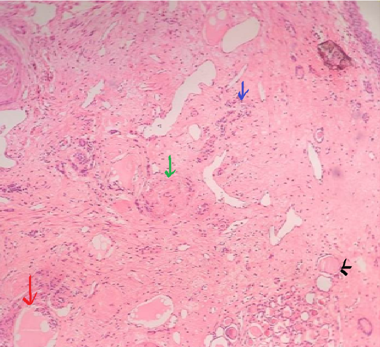
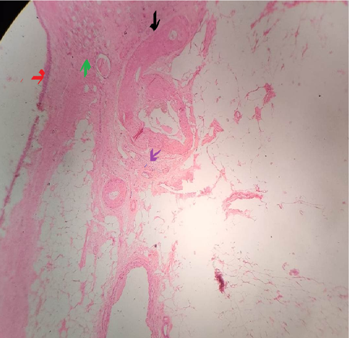
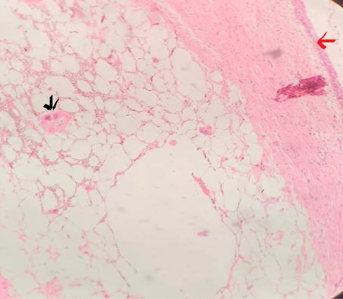
A 72 year-old female patient presented with pain in the left flank region for the past 1 year. Pain was mild, dull and non-radiating. There was no past history of fever. On physical examination non-tender, firm, ill-defined mass in the left renal region was palpated. There was associated hypertension but no history of tuberculosis or diabetes mellitus. Laboratory and radiological investigations done. Urine analysis, Haemogram and Renal function tests all showed results within normal limits. Ultrasonography of left renal region revealed a left hypoplastic kidney. Dynamic renal dimercaptosuccinic acid (DMSA) scan revealed left kidney decreased in size and shape and clearance of the dye with 6% perfusion rate only (Figure 1). The right kidney was normal. A left nephrectomy was performed and left kidney was sent for histopathological examination to our department. Gross examination of specimen showed left kidney with extensive perinephric fat measured 12x5x4cm. On cutting entire renal parenchymal was replaced by yellow adipose tissue with atrophied cortical renal parenchyma and mildly dilated pericalyceal area (Figure 2 a). Cortical thickness is <= 1cm. Multiple tiny stones were present on the replaced adipose tissue (Figure 2b). Slides were prepared and stained with hematoxylin and eosin. Microscopic examination revealed extensive mature adipose tissue replacement in atrophied and compressed renal parenchyma with some sclerosed glomeruli, periglomerular fibrosis, extensive thyroidisation of renal tubules and thickened blood vessels (Figure 3, Figure 4, Figure 5). There was mild to moderate inflammation including lymphocytes and plasma cells. No xanthomatous change was noted. Clear demarcation between mature adipose tissue and renal parenchyma is appreciated. The postoperative period remained uneventful.
Figure 2
Left kidney showing complete replacement of renal parenchyma (2a) Thinned out atrophied renal cortical region (shown by green arrow) and calculi (shown by orange arrow) (2b)
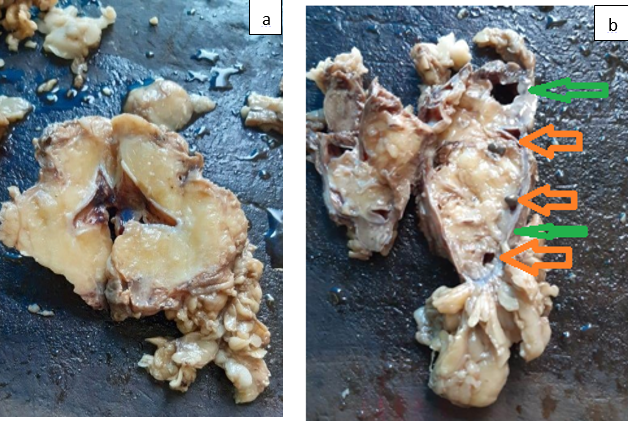
Figure 3
Histomorphology showing atrophy of renal parenchyma (red arrow) and replacement by mature adipose tissue. Sclerosed glomeruli is also seen (black arrow) [4x10]
Discussion
Renal replacement lipomatosis was first described by Kurtzmann in 1931 as reported by Peacock and Balle.4 Renal sinus lipomatosis, replacement lipomatosis, and fibrolipomatosis of kidney are the terms used for this rare condition and represent a spectrum of changes.1 Changes involved in the RRL is the proliferation of mature adipose tissue involving sinus, hilum, and perinephric region along with presence of atrophied renal parenchyma. It is different from renal lipomas in which adipocytes proliferation is in association with normal renal parenchyma.2, 3, 5 Renal sinus lipomatosis, is usually seen in the sixth and seventh decade associated with obesity or use of steroids or idiopathic conditions. It is usually secondary to renal calculus in 70% of the cases and occasionally after renal infarction. However, some RRL cases are also reported in associations with aging, renal tuberculosis and post renal transplantation.6, 7, 8
Usually RRL is unilateral in occurrence and rarely idiopathic.1, 2 It has been observed that its pathogenesis is put under two theories, one suggesting a compensatory mechanism in which the adipose tissue occupies the space that is produced by the atrophied or destroyed kidney and second to compensate renal tissue loss when there is an inflammatory induction of fatty proliferation.2, 5
The presence of atrophic renal parenchyma distinguishes this condition from other causes of fibro-fatty proliferation in and around the kidney, as in obesity, Cushing's disease or excessive corticosteroid therapy and idiopathic.9 It has been reported to occur in transplanted kidneys also. USG shows parenchymal atrophy or a hyper/hypo echoic renal sinus mass with calculi.
Malakoplakia, fat containing tumors such as angiomyolipoma, xanthogranulomatous pyelonephritis, liposarcoma and lipomas may be considered as main differential diagnosis for RRL.2 Xanthogranulomatous pyelonephritis and RRL can occur simultaneously.10 Angiomyolipoma is different from RRl as, it is well circumscribed focal mass of smooth muscle element & with tortuous prominent vessels. In my case such features are not noticed. Liposarcoma is usually located at retroperitoneal extrarenal region. 10 Microscopically well differentiated liposarcoma show lipoblasts unlike in reported case of RRL. Lipoma is excluded by lack of well circumscribed intra parenchymal benign lipomatous mass. Angiomyolipoma is different from RRl as, it is well circumscribed focal mass of smooth muscle element & with tortuous prominent vessels. In my case such features are not noticedXanthogranulomatous pyelonephritis is excluded by absence of xanthoma cells. Pelvic lipomatosis is seen as overgrowth of infiltrative adipose tissue which is non capsulated, non-malignant. It is usually symmetric and limited to the pelvis and rarely to retro peritoneum.11 Pelvic lipomatosis and renal lipomatosis both can present with renal failure, but are totally different entities.
In renal replacement lipomatosis CT scan shows pus filled, dilated calyces and xanthogranulomatous tissue (−15 to +15 HU {Hounsfield units}) reflecting the presence of intracellular fat droplets as against the pure fatty tissue seen.12 CT appears to be the imaging method of choice in RRL, the various CT features include abundant adipose tissue in the renal sinus and perirenal region, marked parenchymal atrophy and calculi. MRI, with techniques of fat suppression can show features similar to CT. Renal liposarcoma is located peripherally (between the kidney and renal capsule), and does not produce a defect in renal parenchyma. In xanthogranulomatous pyelonephritis, CT reveals renal calculi, pyonephrosis, infiltration of adjacent soft tissue or abdominal wall, and parenchymal low attenuation consistent with absecess. 13
Patient may be asymptomatic and can show various features, the usual complaint in literature is flank pain, dull aching, and non-radiating, weight loss, hematuria, fever and palpable mass, some of which were seen in these cases.1, 2, 4, 14, 15 They can also present with complaints of urinary tract infections due to urinary stones or mass in the abdominal cavity. 3 Blood urea nitrogen and serum creatinine is usually within the normal limits4. They are normal if the disease is unilateral with other well functioning kidney. CT scan can confirm the fatty infiltration in the kidney 2 as reported in literature Xanthogranulomatous pyelonephritis and fat-containing neoplasms including lipoma, liposarcoma, and angiomyolipoma are the usual differential diagnosis. CT scan and magnetic resonance imaging scan appear to be an accurate method for demonstrating the distribution of adipose mass within the renal sinus and perirenal space. 2 Histopathology is the appropriate investigation of choice for definite diagnosis and exclusion of other entities.
Conclusion
Focus of the case report is that RRL is a relatively uncommon entity. Histopathologically there is gradual replacement of the renal parenchyma with mature adipose tissue and atrophic features (unlike of Renal Lipoma). Pertains features of poor or non-functioning kidney, show association with chronic calculus diseases, renal tuberculosis or chronic pyelonephritis. Radiologically and clinically it might be confused with neoplastic conditions. CT scan is the investigation of choice to differentiate it from renal neoplasms and histopathology is required for definite diagnosis. Due to lack of experience and paucity of cases, Renal replacement lipomatosis may be under diagnosed if not considered, so we hope for the proper correlation of the case among urologists, radiologists and pathologists, leading to the awareness of the rare entity.