Introduction
Angioleiomyoma, also called vascular leiomyoma or angiomyoma, is a rare benign dermal or subcutaneous tumor composed of well differentiated smooth muscle tumor cells arranged around variable sized vascular channels.1 WHO classified Angioleiomyoma under Pericytic tumor and they recommended that a morphological continuum exists between angioleiomyoma and myopericytoma.1 Angioleiomyoma accounts for 4-5% of all benign neoplasms of soft tissues and commonly present as painful solitary slow-growing nodule on extremity particularly the lower leg.1 In lower extremities Angioleiomyoma occurs two times more common in females than males whereas those occurring in upper extremities or head are more often seen in males than females.1
Although it can be seen at all ages but are more commonly seen between the fourth and sixth decades of life. 1
Case Presentation
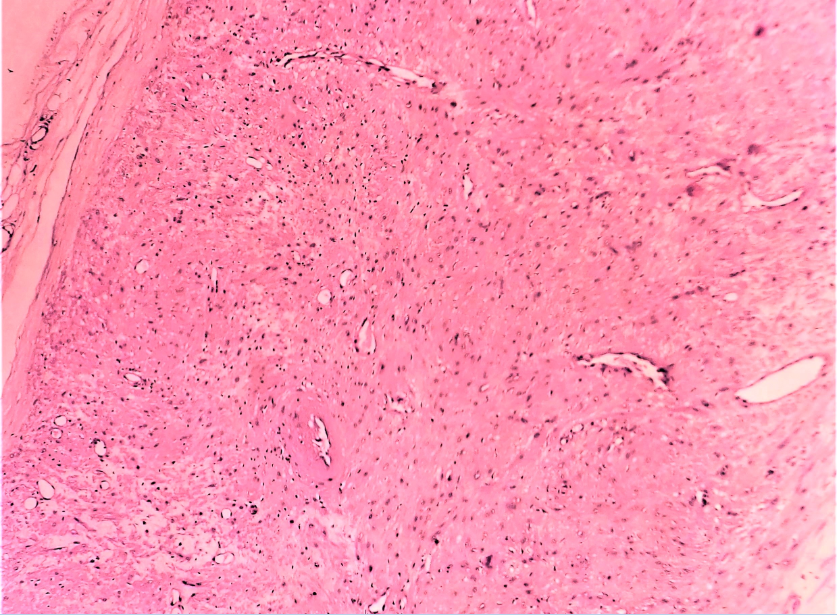
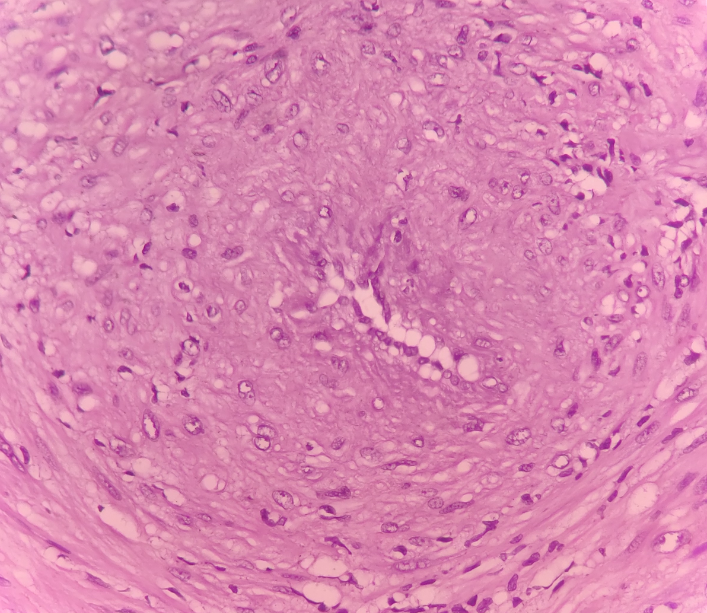
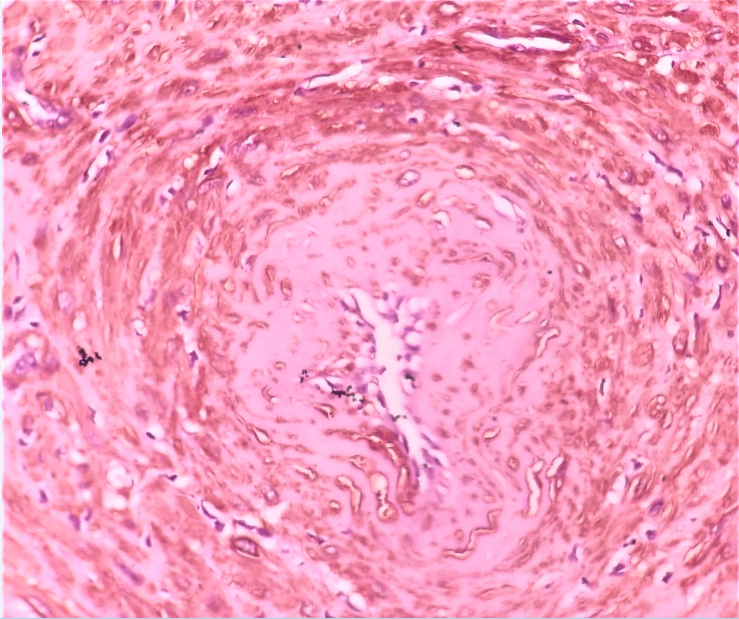
A 30-year-old male came to our hospital with a complaint of painful swelling on left lower leg since six years with progressive increase of swelling to present size. On physical examination, the swelling was soft to firm, tender measuring 2.5 x 2 cm. A clinical diagnosis of sebaceous cyst was made clinically. FNAC revealed paucicellular, haemorrhagic smears with admixed spindle cells singly and in small clusters. Excisional biopsy were performed and sent for histopathological examination. Grossly a single, encapsulated globular tissue piece measuring 2.2x1.5x1.2cm was received in histopathology lab. Cut section of globular tissue was homogenous grey-white with hemorrhagic foci. (Figure 1) Microscopically, sections taken showed a well circumscribed encapsulated lesion composed of fascicles of loosely compacted mature smooth muscle cells surrounding variable sized vascular channels.(Figure 2, Figure 3) The cells were bland slender to plump with scanty eosinophilic cytoplasm and regular nuclear outline. Focal areas of haemorrhage was also seen. No atypia, necrosis or atypical mitosis was noted. Immunohistochemical stain for smooth muscle actin (SMA) revealed diffuse strong membranous and cytoplasmic positivity in the perivascular smooth muscle cells. (Figure 4). Thus a final diagnosis of Angioleiomyoma of left lower leg was rendered.
Figure 1
Gross Examination: Cut section of the excised mass show homogenous grey-white area with hemorrhagic foci.

Discussion
Superficial Leiomyoma of skin and subcutaneous tissue are mainly of three types (i) Piloleiomyoma: arises from arrector pili muscle, (ii) Angioleiomyoma: arises from smooth muscles of the blood vessels and (c) Genital leiomyoma: arises from the smooth muscles of nipple, vulva and scrotum).2 Angioleiomyomas are rare subcutaneous or deep dermal benign tumors of smooth muscle of blood vessels. The etiology of these tumors remains unknown but trivial trauma, venous stasis, hamartomatous changes, arteriovenous malformations and hormonal imbalance especially of oestrogen have been related as potential causal etiology of the tumor.3 Association with EBV has been seen in immunocompromised patients with angioleiomyomas or other smooth muscles tumors.3 These lesion can occur anywhere in the body however they are most commonly noted in extremities particularly lower leg followed by head and trunk. 1 The lesion is commonly located in subcutis and sometimes in deep dermis. Rarely they may be presented as subfacial or intraosseous lesions. 1 Extremely rare sites of angioleiomyomas in external auditory canal has been reported by Picciotti et al4 and in orbit by Alam et al.5
Angioleiomyomas presents as small slow growing painful firm rubbery nodule. The pain is typically described as paroxysmal provoked by exposure to pressure, cold, pregnancy or menstruation.1 Grossly, most angioleiomyomas are well circumscribed grey white or grey brown nodular lesion typically less than 2 cm in diameter. Histopathological findings show well differentiated smooth muscle cells with intervening vascular channels. Common histological variations of angioleiomyoma include solid, venous and cavernous types.6 In a study of 562 cases solid type pattern (67%) was most commonly observed by Hachisuga T et al.7 Secondary changes like calcification, myxoid degeneration, hyalinization, and malignant transformation have been reported. The dystrophic calcification has been reported to occur due to minor pressure, an injury, a previous inflammatory process, or de novo.8 Mitotic figures are absent or rare. The tumor cells show strong and diffusely positivity for SMA, MSA, Calponin, desmin and sometimes variably for h-caldesmon while being negative for HMB-45.9
Standard treatment includes marginal surgical excision of the tumor. Local recurrence or malignant degeneration after surgical excision is rare. Owing to the ambiguous nature of the clinical findings, angioleiomyoma should be included in the differential diagnosis of lower-extremity soft-tissue manifestations. Painful subcutaneous lesions of the extremities such as hemangioma, angiolipoma, ganglion cysts, glomus tumor and traumatic neuroma should be considered for differential diagnosis.10 There should be an increased index of suspicion for angioleiomyoma, especially when a freely mobile subcutaneous mass is encountered particularly in a young patient.
Conclusion
Angioleiomyoma is an infrequent soft-tissue tumor of pericytic origin, with a nonspecific presentation. It should be considered in the differential diagnosis of deep dermal or subcutaneous swellings, especially in the extremities. Excision of the lesion leads to complete resolution of symptoms, and histopathology gives a definitive diagnosis.