Introduction
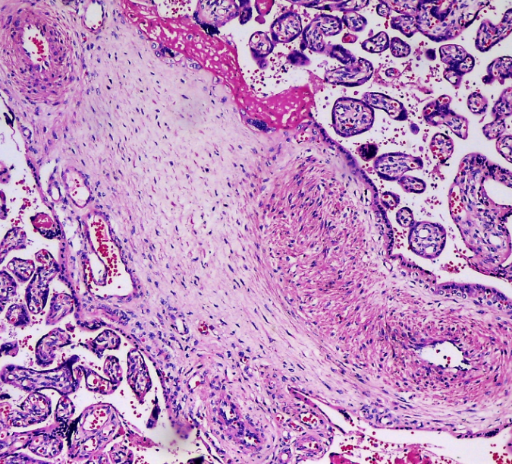
Placental mesenchymal dysplasia(PMD) is a rare clinicopathologic entity characterized by placentomegaly and USG features of grape like vesicles resembling partial mole.1 The gross findings of abnormally enlarged placenta with dilated or aneurysmal blood vessels with histologic evidence of edema of the stem villi and thick walled blood vessels and characteristic absence of trophoblastic proliferation is suggestive of PMD.2 This entity was first described by Moscoso et al. in 1991 as stem villous hyperplasia.3 The true incidence of PMD is unknown, but is estimated to be around 0.002 - 0.02%.4
Case Report
A 28 years old second gravida was referred to our hospital with high blood pressure and USG features of oligohydraminos and abnormal doppler.
Her last childbirth was Lower Segment Caeserian Section 4 years back, due to meconium stained amniotic fluid. She delivered a 3.4kg female baby. The postoperative period was uneventful.
On examination, she had a pulse rate of 82/ minute and BP: 140/110 mmhg. She was afebrile and had bilateral pedal edema.
Her investigations showed Hb:11.9gm/dl, Total count: 11400/mm3, Platelets:3.2 lakhs/mm3. Her Liver function test was normal except for an elevated LDH of 581 IU/L. Her urine examination showed presence of albumin.
A repeat ultrasound done in our hospital showed a cephalic, single live intrauterine gestation of 30 weeks with a large placenta of 14cm thickness and cystic spaces within. She had severe oligohydraminos with restricted fetal movements. The expected fetal weight was 1.54kg.
She was posted for emergency LSCS in view of severe preeclampsia at 33 weeks and 4 days. She delivered a female baby weighing 1.29kg with an APGAR score of 8 at one minute and 9 at five minutes.
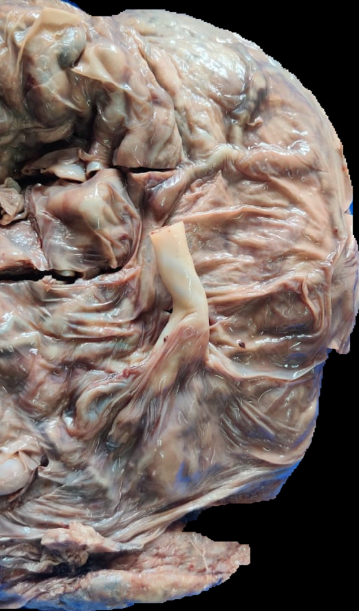
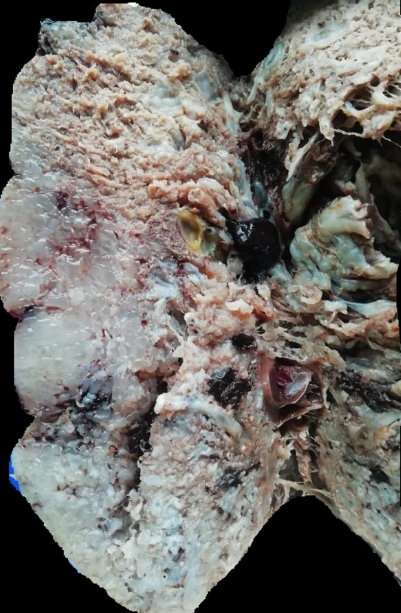
We received her placenta for histopathological examination. Placenta was abnormally large and weighed 1.4 kg with a thickness of 8cm. The fetal surface showed multiple engorged vessels with a normal umbilical cord showing two arteries and one vein. Cut section showed multiple cystic spaces, myxoid areas and numerous blood vessels. Microscopy showed edema of the stem villi with numerous thick walled blood vessels. The terminal villi were normal and there was no trophoblastic proliferation.
USG of the newborn showed a well defined multicystic lesion in the segment VIII of liver, measuring 3.7 x 3.4cm, with internal septations of maximum thickness 1.5mm, consistent with mesenchymal hamartoma.
On follow up, the mother is doing well and a repeat ultrasound of the baby at 6 weeks showed a reduction in the size of the hepatic lesion. The child is hence now under conservative management.
Discussion
PMD is a benign vascular malformation, the etiology of which is currently unknown. The speculated theory is that PMD is a congenital malformation of the mesoderm.5 There is no specific clinical symptomatology associated with PMD. PMD usually involves a normal fetus, but can be associated with intrauterine growth restriction, still birth and Beckwith Weidmann syndrome in a significant number of cases.6 Abnormalitites of umbilical cord, like long, twisted and tortous cords also have been reported.7
Hepatic mesenchymal hamartomas are characterized by benign proliferation of the mesenchymal liver tissue. Although rare in combination with PMD, it is known to have a poor prognosis than foetuses without structural abnormalities.4
PMD is usually considered as a differential diagnosis of other placental lesions which are usually multicystic, like chorangioma, molar pregnancy, subchorionic hematoma and spontaneous abortion with hydropic changes in the placenta. A normal karyotype and lack of high velocity signals inside the lesion favours a diagnosis of PMD.2 The closest differential is molar pregnancy and it is significant to differentiate the two entities in view of changes in manangement and outcomes.