Introduction
One of the hallmark of well-being of newborn infant is timely passage of first stool. Intestinal obstruction is suspected in any full-term infant who does not pass meconium in first 24 hours of life and in premature infants who have excessively delayed passage of meconium (i.e 7-8 days).1 Proximal obstruction like esophageal/gastroduodenal atresia presents earlier than distal obstruction while functional obstruction i.e Hirschsprung’s disease may present later. Incidence of small intestinal atresia is 1 in 5000 newborn infants. Other causes of intestinal obstructions are Annular Pancreas, Meconium ileus, Malrotation, Peritoneal band, Meckel’s Diverticulum, Mesenteric cysts, Intussuception, Hirschsprung’s disease, Strangulated inguinal hernia or diaphragmatic hernia.2 The etiology of jejunoileal atresia is postulated as consequence of an intra-uterine mesenteric vascular accident secondary to volvulus, incarceration in a prenatal umbilical hernia, or intussusceptions.3, 4 The purpose of this case is to detail about the histopathological features of neonatal small intestinal atresia and review of literature.
Case Report
A Full term (38.2 weeks) male baby delivered through LSCS. Liquor was clear, Apgar score was 7, 8, 9 at 1min, 5 min and 10 min respectively. Urine passed in < 8 hours after birth. Baby had not pass meconium even after 24 hours and baby presented with distension of abdomen. Nasogastric tube showed bilious aspirate. On examination temperature was normal, cried, activity good, HR: 140/min, RR: 46/min SPO2-96%. Abdomen was soft, mild distended; non-tender, anal opening was patent. Other organs were normal.
Radiological Studies: Antenatal scan of mother at gestation age of 34 weeks 1 day showed dilated colon measures 2.2 cm in diameter. Target sign seen at anal canal. Hirschsprungs Disease was suspected on antenatal ultrasonography findings. Post natal after day 1 of birth X-ray abdomen showed multiple air-fluid levels in abdomen with dilatation of small bowel loops suggesting distal small bowel mechanical obstruction. Invertogram showed gaseous distention of small bowel loops with air fluid levels. No gas seen in large bowel, rectum and anal canal. On Contrast barium enema there was free flow of contrast through rectum, sigmoid colon, descending and transverse colon with minimal distention of colon (microcolon). There was no evidence of stricture, stenosis or abnormal dilatation of visualised colon. There was no evidence of malrotation or abnormal rotation of large bowel.
Patient was operated under general anaesthesia with supraumbilical incision, abdominal wall was opened up in layers. The abdominal cavity showed dilated ileum with ceacum, small intestinal atresia was noticed at ileocecal junction, colon appeared normal. The dilated ileum 10 cm above the atretic end along with ceacum was resected and end to end anastomosis done and sutured in layers. The specimen was send to histopathology lab for examination.
The labelled resected specimen was received at Department of Pathology for histopathological examination. Specimen was labelled as ileocecum with appendix; the entire segment measured 10cm in length. It was cut opened along antimesentric border and meconium was drained out and specimen was fixed in neutral buffered formalin for 8 hours.
On gross examination it showed an intact imperforated thick membrane 1.5 cm from distal resected margin, obstructing the lumen at the junction of ileum and ceacum. Thickness of membrane was 1.5 mm. The lumen of segment proximal to the membrane was dilated mucosal folds were intact and wall appeared thinned out. No ulceration, congestion, no diverticuli seen. Caecum with appendix measuring 4.5cm in length appeared unremarkable.
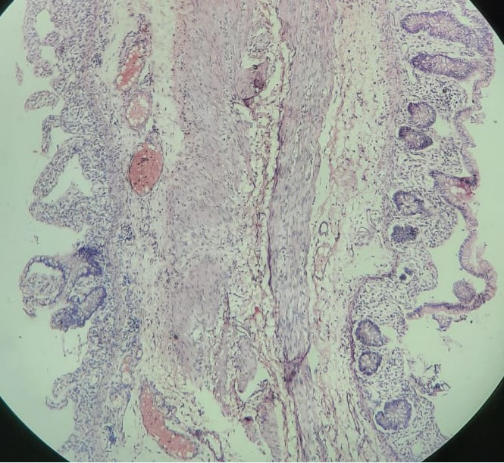
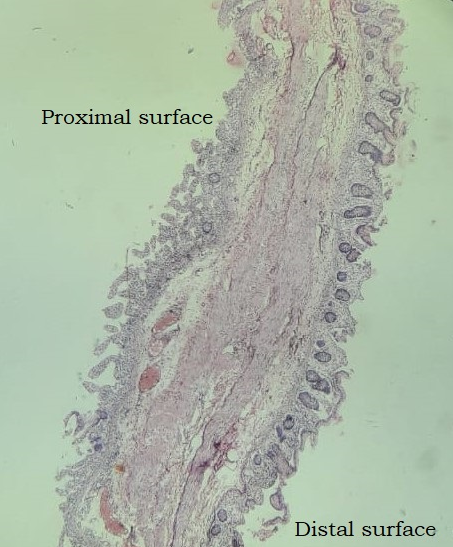
Detailed microscopic examination of ileal sections revealed mucosal and submucosal oedema along with presence of ganglion cell within the mucularis layer. Serosa showed congested blood vessels. Section from the membrane showed attenuated mucosal layer with flattening of villi and ulceration, submucosa showed congestion and mononuclear cell infiltration. Section from caecal end showed flattening of villi and mucosal and submucosal oedema, muscularis propria shows ganglion cells. Section from appendix was unremarkable. Histological findings were suggestive of Type 1 Septal Intestinal Atresia.
Discussion
Intestinal atresias account for one third cases of neonatal intestinal obstructions. It can be small intestine which accounts for majority of cases than colonic atresia. The distal portion of ileum is most commonly involved.5 In our case similarly distal ileum was involved. Neonates with ileal atresia have fewer congenital anomalies associated than duodenal atresia and colonic atresia upto 75% of colonic atresia are found proximal to splenic flexure usually in the ascending colon with significant amount of colon missing in most infants.6 This is commonly associated with other anomalies, which include abdominal wall defects, abnormality of the genitourinary tract, anal atresia, imperforate anus, Hirschprung’s disease, omphalocoele, absent hand, cleft lip and palate, facial asymmetry and bilateral optic nerve atrophy.6 In our case there was no associated congenital anomaly. The mean age of presentation was 2.2 Days and our case presented on Day 2. The etiology of small intestinal atresia differs with its site of origin.7 Since excretion of bile begins about the eleventh week and squamous epithelial cells swallowed from the vernix caseosa are found in the intestine after the twelfth week, the presence of these elements in the intestinal lumen distal to any level of congenital atresia would indicate that occlusion occurred sometime after the eleventh or twelfth week of fetal life, well beyond the period of development of the intestinal tube.8 Furthermore, the segmental absence of the jejuno-ileal mesentery cannot be accounted for on the basis of a failure of recanalization. A more plausible explanation is that jejunoileal atresia is a consequence of an intra-uterine mesenteric vascular accident secondary to volvulus, incarceration in a prenatal umbilical hernia, or intussusceptions.3, 4 More proximal the mesenteric vascular compromise greater the resulting severity of the intestinal atresia. The extent of these changes depends upon the time of development of the obstruction as well as the site of involvement. The spectrum of histological features depends on extent, severity and duration of an ischemic event. The mucosa and submucosa is more susceptible to ischemic injury than muscularis. Injury to full thickness of the bowel may result in perforation and meconium peritonitis. If the ischemic segment undergoes healing rather than perforation, there may be scarring of mucosa, submucosa and muscularis leading to stenosis or atresia.9 Small intestine atresia are classified using Martin & Zerella’s.7 and Louw’s classification,8 as: Type I: Septal Atresia. Type II: Fibrous cord joining atretic ends. Type IIIa (Louw’s): Atretic ends separated by V shaped mesenteric defect. Type IIIb: Multiple atresias Type IV: Apple peel atresia. Type II is the most common form. Our case was of Type I Small intestinal atresia with Septal intestinal atresia. The histological features observed in our case like flattening of villi, mucosal and submucosal oedema, congestion and vascular proliferation in serosa suggest that the affected infant was suffering from intrauterine intestinal ischemia contributing to the development of atresia. Moreover presence of lanugo, squames, and meconium distal to an atretic segment (Santulli and Blanc, 1961)10 or segments of atretic bowel separated by relatively normal bowel and presence of meconium (Schultz and Lawrence, 1960) explains ischemia is an aetiological factor rather than failure of recanalization.11 Pandey A et al study found that functional intestinal obstruction being most common cause of post operative complication cause believed to be ineffective peristalsis due to grossly dilated atretic segment. Hence they concluded that the bowel proximal to the atresia is abnormal for a varied length at least up to about 10 cm proximal to atresia.12 Similarly in our case dilated ileum was resected 10 cm proximal to atretic end with end to end anatomosis.
Conclusion
Intestinal Obstruction is an emergency encountered in newborn infants requiring early accurate diagnosis by radio imaging modalities. Spectrum of histological findings like flattening of villi, ulceration, and prominent vascular proliferation can be seen in intestinal atresia. Histopathological examination is important in these cases in order to rule out other abnormalities (Hirshsprung’s disease) and also to assess presence of segmental intestinal musculature defect which can lead to post operative functional obstruction.