Introduction
Sex cord tumor with annular tubules (SCTAT) is an unusual sex cord stromal tumor (SCST) accounting for approximately 2.3% of SCST and 8% of all primary ovarian neoplasms.1, 2 It is composed of both granulosa cell and sertoli cell elements.2 Majority of patients with SCTAT present usually during reproductive age. SCTAT can be associated with Peutz-Jeghers syndrome (PJS) in 1/3rd of the patients, which can be seen in all age groups. Mean age is 27 years. In syndromic cases, the tumors usually involves both the ovaries, at more than one focus and are clinically benign. The tumor is usually unilateral, unifocal, large in non-syndromic form and 15-20% of cases tend to be clinically malignant and hence warrants a long term follow up of such cases.3
Case History
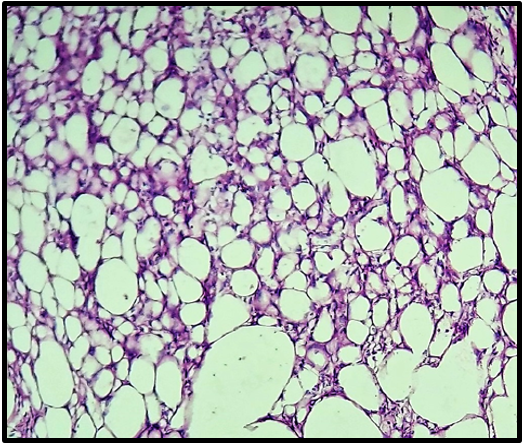
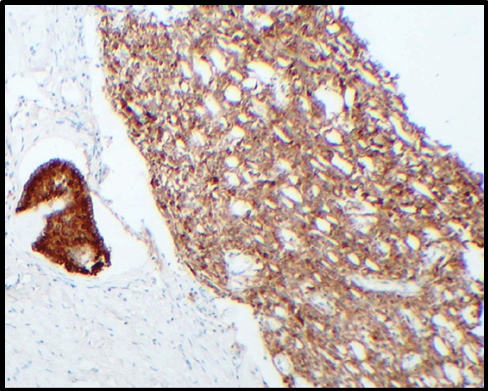
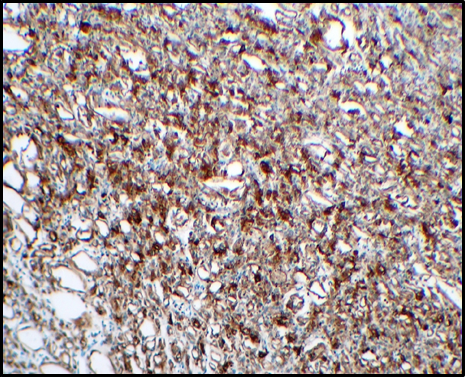
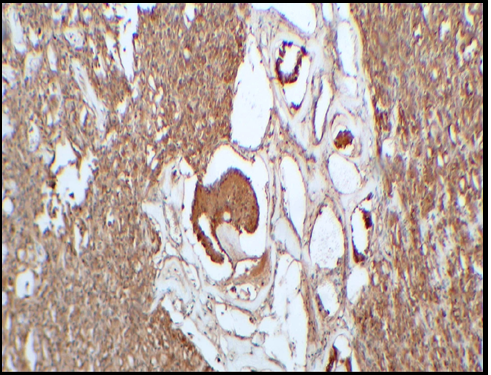
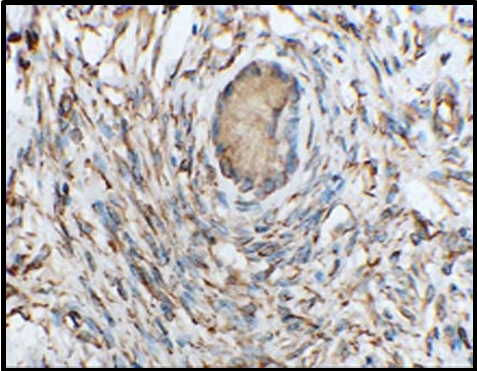
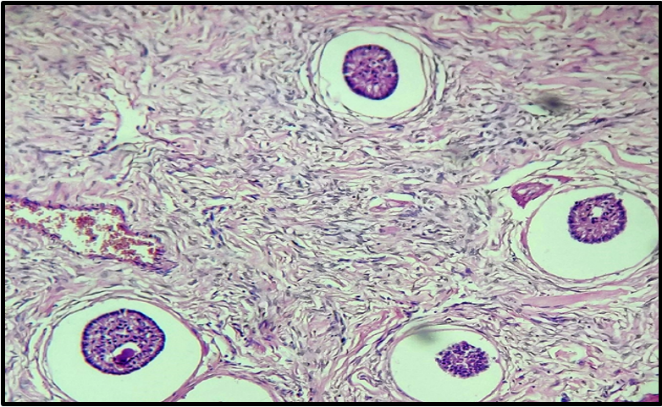
A 23 year old unmarried female presented with pain abdomen and mass per abdomen. Ultrasonography revealed a left adnexal mass of size 19x14x11cm. A differential diagnosis of teratoma/ dysgerminoma was given. Intraoperatively a large left ovarian mass with complete torsion yet maintained vascularity and tube stretched over it was noted. Left salpingo-oophorectomy was performed and sent for histopathology study. Gross examination revealed a large, grey-white, smooth, globular mass measuring 12x9x3cm with attached fallopian tube [Figure 1]. Cut section showed variegated appearance with solid and cystic areas [Figure 2]. On microscopy, many simple and complex hyalinised annular tubules were seen, surrounded by basement membrane like material in few tubules [Figure 3] Complex tubules show paired cell arrangement with palisading of nuclei and core of eosinophilic hyaline material. The tumor cells in tubules are columnar having clear to eosinophilic cytoplasm with round to oval nucleus showing mild to moderate anisonucleosis, inconspicuous nucleoli and some showing nuclear grooves. At places tumor cells were arranged in nests, microcystic and solid pattern. Foci of sertoli cell and granulosa cell differentiation was seen [Figure 4]. Based on these findings, a diagnosis of Sex cord tumor with annular tubules was made. Immunohistochemistry (IHC) was done which showed immunoreactivity of tubules for alpha-inhibin [Figure 5], pancytokeratin [Figure 6], calretinin [Figure 7], vimentin [Figure 8] and negative for CD10. IHC study confirmed the histopathology diagnosis.
Figure 4
Microphotograph 100X magnification H&E stain: sertoli cell & granulosa cell differentiation, hyalinised stroma
Discussion
SCTAT was first described by Scully in 1970 for a peculiar form of ovarian neoplasm.1, 2, 3, 4 The SCTAT is composed of aggregates of simple or complex ring-like, tubular structures with fibrous stroma. The tumor cells are columnar with clear or foamy cytoplasm and round to oval hyperchromatic nuclei. Foci of granulosa cell or sertoli cell differentiation are not uncommon.4 Electron microscopy of tumor cells has revealed Charcot-Bottcher filaments which are characteristic of sertoli cells.5 Differential diagnosis includes sertoli cell tumor, gonadoblastoma and microfollicular granulosa cell tumor.6 SCTAT shows immunopositivity for inhibin, calretinin, pancytokeratin, vimentin, WT1 and are negative for EMA, CD10.5, 7
In the present case also tubules were positive for calretinin, pancytokeratin, vimentin and were immunoreactive for inhibin. These findings helped in the indexed case to confirm the diagnosis of SCTAT. As SCTAT secretes estrogen and progesterone, the clinical manifestations like isosexual precocity, menstrual irregularity and post-menopausal bleeding may be seen.4 However clinical manifestations of estrogen and progesterone secretions were not observed in the present case. Thorough clinical examination of the patient did not reveal any features suggestive of PJS such as benign hamartomatous polyps in the gastrointestinal tract or hyperpigmented macules on lips and oral mucosa.4 Hence the present case was concluded as non-syndromic SCTAT and was suggested close follow up as risk of malignancy is high in non-syndromic cases.
SCTAT has histopathological features of a benign tumor but can recur and metastasize later in life and hence SCTAT is now recognized as low-grade malignancy. Yet it has a favourable prognosis despite its high rate of recurrence. Patients complaint of menstrual disturbances or present with abdominal or pelvic masses again at the time of recurrence.1 Hart first documented the metastatic potential of SCTAT and speculated the metastasis was via lymphatic vessels.4 Tumors that recur are usually located in retroperitoneal region involving mainly para-aortic lymph nodes. Supraclavicular lymph nodes and other organs like liver, lung, kidneys, peritoneum & omentum may be involved in advanced cases.8 The duration ranges from 3 months to 20 years for first time recurrence of SCTAT as reported by Kulkarni.9 Serum estradiol and progesterone levels can be done to monitor progression or regression of the tumor.1
Clinical management includes surgical removal of the tumor. Preserving fertility should also be considered because majority of the cases present during adolescent period or in reproductive age group. 1 Ovarian cystectomy can be considered depending upon tumor size, patient’s age and need to preserve ovarian function for future fertility. However the risk of recurrence of tumor has to be weighed in cystectomy patients.7 A study done by Yinon et al10 found no statistically significant difference in rates of tumor recurrence between patients who underwent unilateral salpingo-oophorectomy versus ovarian cystectomy. Whereas a study done by Qian et al1 showed high rates of tumor recurrence in patients who underwent ovarian cystectomy. Owing to complete involvement of affected ovary, unilateral salpingo-oophorectomy was done and the other ovary was preserved in our case. As SCTAT are tumors of rare occurrence, standard treatment protocols are yet to be established.1, 6
Conclusion
SCTAT are uncommon tumors with distinctive morphologic pattern. Thorough clinical examination is warranted to determine PJS. Considering the young age of the patient and chances of tumor recurrence later in life, a proper counselling for long term follow up is very essential in non-syndromic cases like that of ours.