Introduction
Cytological study of body fluids is an important diagnostic test. It should be judiciously used for cases where there is a strong clinical suspicion for malignancy. In many cases, cytology with adequate clinical information can lead to a conclusive diagnosis. Pleural fluid cytology is widely recognised and well documented, however peritoneal fluid cytology needs better understanding and documentation. The cytological study of peritoneal fluid is of paramount importance in indicating accurate diagnosis. Presence of malignant cells in the peritoneal fluid is mostly considered as definitive diagnosis. The positive peritoneal fluid with or without known primary, often connotes advanced carcinoma. It is vital to identify malignant cells accurately and to identify the type of tumour and primary site of origin. The most common challenge here is to distinguish reactive mesothelial cells from malignant cells. Thus, meticulous screening to differentiate the two is required. Cytological study using cytospin smear is usually the first line of investigation in suspected malignant cases. However, cell block is also considered an important diagnostic tool in detecting malignancy. It was Quencke in 1882 who first described cancer cells in abdominal and pleural fluids and Bahrenburg in 1896 was the first to introduce cellblock technique. Cellblock is a simple, rapid and inexpensive method, which can be used to complement the cytological smear. The advantage of cellblock is that the residual material left behind in cytocentrifuge can also be used in cellblock method. Cellblock tissues can also be preserved for future reference. 1, 2, 3, 4
The aim of this study is to (1) analyse the cytomorphology of peritoneal fluid using cytospin and cellblock technique and (2) to assess the utility of cellblock method in identifying malignant cells in peritoneal effusion and wash samples.
Materials and Methods
This was a one-year prospective study conducted in the department of pathology in a tertiary care hospital. The sample size was calculated using the formula N=4pq/L2. A total of 53 peritoneal fluid samples which included both ascitic fluid and intraoperative peritoneal wash samples were received by the department that were clinically suspicious for malignancy. Paracentesis and peritoneal wash were performed by the clinician with informed consent from the patient and under aseptic precautions. The aspirated fluid was collected in a clean container and sent unfixed to the laboratory immediately or otherwise stored at 4℃ for 24-48 hours. On receiving, the sample was appropriately labelled and gross examination of the sample was carried out. Container was shaken to disperse the cells and a 50ml aliquot of fluid (the first part or the entire specimen if less than 50ml) was placed in a cytospin funnel with filter paper placed between slide and funnel and then centrifuged at 2000 rpm for ten minutes. Smears formed were then fixed in 95% alcohol and stained with Hematoxylin and Eosin stain and Papanicolaou stain and examined under microscope. Unfixed smears were stained with Leishman stain. Whenever required, special stains like Periodic acid Schiff (PAS) and Alcian blue was used. The remainder of the sediment (second part) was mixed with two to three drops of plasma. Then two to three drops of thromboplastin reagent was added and mixed. Later, ten percent buffered formalin was added and kept for fixation for 30 minutes. Sediment was then wrapped in filter paper, placed in cassette, embedded in paraffin and cut and stained in the manner of histologic sections. If a clot was found in the sample, it was removed and placed in cassettes for processing as cell block material. Ascitic fluid samples without clinical suspicion of malignancy were excluded from the study. Institutional ethical clearance was obtained for conducting the study.
Statistical analysis
The data collected was tabulated and analysed by proportions and percentages. Descriptive statistics was applied to draw conclusions. Statistical Package for the social sciences (SPSS) version 20.0 software is used to analyse the data. Statistical test like sensitivity, specificity, positive and negative predictive value and diagnostic accuracy were calculated.
Results
In this study, 206 fluid samples including both ascitic fluid and peritoneal wash were received. Among these, only 53 cases (37 ascitic fluid and 16 peritoneal wash) were clinically suspicious for malignancy. Age of the patients ranged from 28 years to 73 years. The mean age was 58±13years.
Cytospin and cell block was performed in all these 53 cases. Twenty six of 53 cases (49.06%) were positive for malignancy and 27 cases (50.94%) were negative for malignancy. Majority of the patients positive for malignancy were in sixth decade (7 cases, 26.92%) followed by seventh decade (6 cases, 23.08%). Female preponderance with 19 (73.08%) females and 7 (26.92%) males was noted. Female to male ratio was 2.7:1. (Table 1)
Physical examination of only Ascitic fluid (22 samples) was performed as the inherent process of peritoneal washing alters the colour and appearance of the sample. Majority of the ascitic fluid samples with positive cytology were yellow (63.6%) in colour followed by red (36.4%). Many of these samples were turbid (72.7%) followed by haemorrhagic (22.7%). Clot was present in 36.4% cases. (Figure 1)
On cytospin, among these 53 clinically suspected malignancy cases, only 25 cases (47.17%) were diagnosed as positive for malignancy, 27 cases (50.94%) were diagnosed as negative for malignancy and one case (1.89%) was considered suspicious because of low cellularity and doubtful morphology on cytospin smear. (Table 2)
Whereas on cellblock, 26 (49.06%) of 53 suspected cases were diagnosed as positive for malignancy. A case which was considered suspicious on cytospin smear was confirmed as malignant on cell block study. The increased diagnostic yield in picking up malignant cell was 3.85%. On the other hand, only 22 (41.51%) of 53 cases could confirm as negative for malignancy on cellblock. Remaining 5 cases (9.43%) which were diagnosed as negative for malignancy on cytospin showed sparse cellularity or no cellularity to opine any confirmatory diagnosis on cell block. (Table 2)
Smears from cytospin method with cell block method were correlated and the results were analysed. Majority of the cases (10 cases, 38.46%) had ovary as the primary site followed by 4 cases (15.38%) of colorectal carcinomas, 3 cases (11.54%) of carcinoma stomach, 2 cases (7.69%) of endometrium, one case (3.85%) of lung carcinoma and one case (3.85%) of synchronous high grade serous carcinoma of peritoneum with well differentiated adenocarcinoma of fallopian tube. For 5 cases, though the smear and cellblock showed malignant cells, the primary tumour could not be detected. (Table 3)
While the most common primary tumour among female patients was ovarian malignancy, among male patients it was colorectal carcinoma. Adenocarcinoma was the most common type of tumour observed in this study. On microscopy, the predominant architectural pattern observed in both cytospin and cellblock was small to large clusters with formation of 3D balls (50%). Other commonly found pattern were papillary architecture (23.08%) followed by tumour cells in singles (15.38%), in sheets (7.69%) and in glandular pattern (3.85%). (Figure 2)
Cytological test showed sensitivity of 96.15%, specificity of 100%, positive predictive value of 100%, negative predictive value of 96.42% and diagnostic accuracy of 98.11% in detecting malignancy. Additional yield for malignancy was 3.85% with cellblock when compared to cytospin smear.
Table 1
Age and gender distribution of cases with positive cytology
Table 2
Cytospin versus cellblock
Table 3
Primary site for metastatic effusion
Table 4
Comparison of common primary tumour in peritoneal fluid
|
Study |
Cytology positive |
Most common primary tumor |
Second common primary tumour |
||||
|
|
|
Site |
No |
% |
Site |
No |
% |
|
Present study |
26 |
Ovary |
10 |
38.46 |
Colorectal |
4 |
15.38 |
|
Ayantunde AA et al 5 |
150 |
Ovary |
44 |
29.33 |
Colorectal |
31 |
20.66 |
|
Karoo ROS et al 6 |
48 |
Ovary |
41 |
85.41 |
Lymphoma |
3 |
6.25 |
|
Chakrabarti PR et al 7 |
46 |
Ovary |
29 |
63.04 |
Gall bladder |
5 |
10.8 |
|
Udasimath S et al 3 |
13 |
Ovary |
5 |
38.46 |
Colon, liver, cervix, bladder |
1 each |
7.6 each |
|
Jha R et al 8 |
21 |
Stomach |
6 |
28.57 |
Ovary |
5 |
23.81 |
|
Bjelakovic G et al 9 |
27 |
Gynaecological |
10 |
37.3 |
Stomach |
4 |
14.81 |
Discussion
The cytological examination of body fluid is gaining importance because the positive fluid is always definitive. It not only helps in detecting the primary but also in staging and prognosis of the disease, obviating surgery, planning radiotherapy or chemotherapy accordingly. Presence of malignant cells in the effusion is almost always conclusive of metastasis, as a primary tumour arising from mesothelial cell lining is very rare. Both cytospin and cellblock are important diagnostic tool in cytology. However, cell block has the advantage of viewing the slide like a histopathology section. Cells can be concentrated in a small area that can be glimpsed at once. Histological patterns can be appreciated and the background is usually clear unlike the smear which can have bloody or dirty background. Multiple sections can be taken and can be used for special staining and immunohistochemistry whenever required. The major benefit is the preservation of slide for a longer duration. Zemansky in 1928 had concluded that cellblock is a superior technique compared to the smear.2, 3
Malignant cytology was noted more in females similar to studies by Karoo ROS et al6 and Grandhi B et al.10 Ovarian malignancy was the most common primary tumor in females and colorectal carcinoma was the most common primary tumour in males. Ayantunde AA et al,5 Karoo ROS et al,6 Chakrabarti PR et al,7 Grandhi B et al10 and Udasimath S et al3 in their respective study have also observed that ovarian neoplasm was the most common primary tumour in peritoneal effusions. On the other hand, Jha R et al8 observed that gastric malignancy (28.57%) was the most common primary tumour in their study but among female patients, ovarian malignancy (23.81%) still remained the most common primary tumour in their study. (Table 4) Joshi A et al11 also opine that most of the cases of malignant peritoneal effusion in their study was due to GI and Ovarian malignancies.
Predominant architectural pattern noted in our study were 3D cluster (50%), followed by papillary pattern (23.08%), singles (7.69%) and glandular pattern (3.85%). Adenocarcinoma was the most common type of tumour observed in this study. Similar observation noted in studies by Chakrabarti PR et al7 and Jha R et al.8
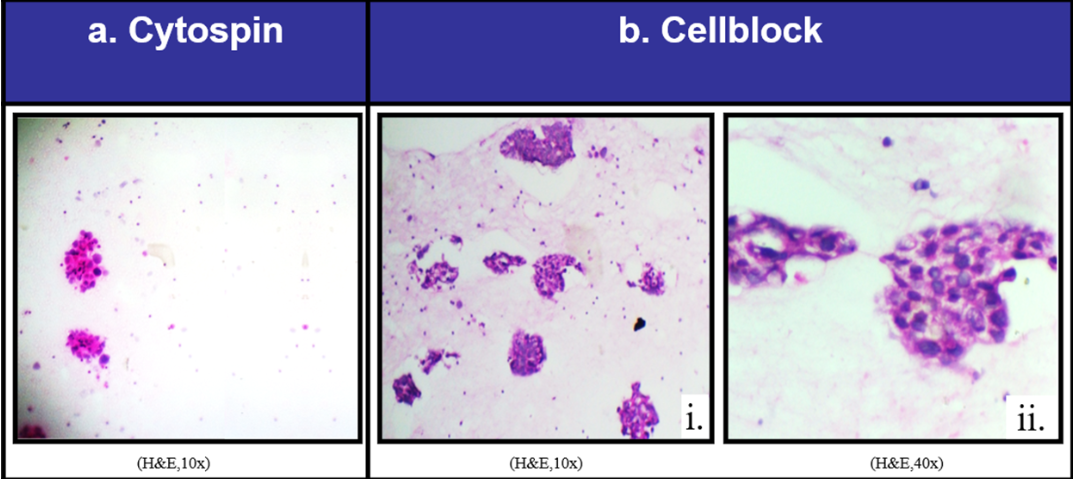
One case of clinically suspected uterine malignancy was considered suspicious for malignancy on cytospin but could not confirm malignancy due to low cellularity and presence of very few atypical cells in the smear. This case was confirmed as positive in cellblock due to concentration of cell and clear malignant picture. (Figure 3) Additional cellular yield was noted by cellblock in detecting malignant cells which was in line with the studies done by Shubada B et al,1 Viral MB et al4 and Gayathri MN et al.2
Figure 3
Uterine malignancy, Case of clinically suspected uterine malignancy (1): Photomicrograph of cytospin smear showing low cellularity with occasional cell clusters comprising of a few atypical cells. Suspicious (H&E, 10X). (2): Photomicrograph of cell block, (i): Showing high cellularity with tumor cells in glandular pattern and small clusters. Positive for malignancy (H&E, 10X), (ii): Showing tumor cells in a cluster with large hyperchromaticnuclei (H&E, 40X).
In cases that were positive for malignancy, cellblock not only increased cellularity but also showed better morphological detail. Different architectural patterns with better nuclear cytoplasmic particulars could be appreciated compared to cytospin smears contributing to the increased diagnostic yield.
There were 5 cases (9.43%) diagnosed as negative for malignancy on cytospin and on correlation with clinical detail, but on cellblock no opinion could be formed. The reason for this being sparse cellularity or no cellularity to opine any confirmed diagnosis on cell block. This could be due to loss of material during processing and preparation of cellblock. However, cytospin smears of these samples showed clear morphology due to evenly distributed cells.
The above observations points out that, cellblock usually helps in picking up the malignant cells due to concentration of cell in smaller area and increasing the diagnostic yield and cytopsin smears helps in studying the morphology of other non malignant cells due to their even distribution in the smear. Cytospin smears are no doubt a good method for cytodiagnosis, but cellblock can give additional information complimenting the diagnosis especially in detecting malignant cells.
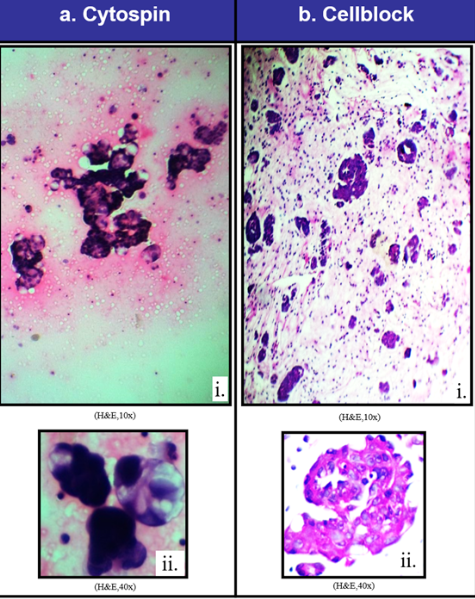
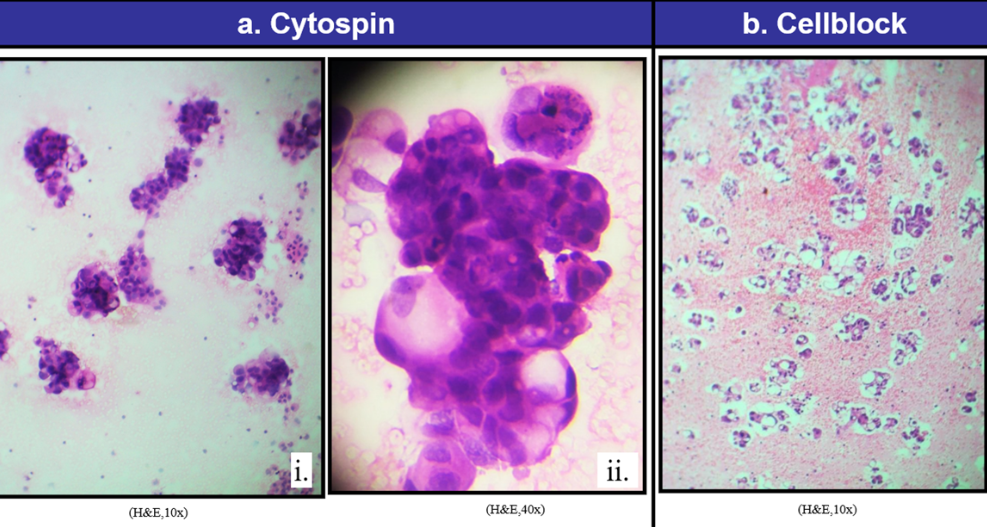
In the present study, one case of ovarian malignancy on cytospin of peritoneal fluid showed tumor cells in papillae and 3D clusters. Cellblock of the same showed tumor cells arranged in papillae, cords and clusters. The tumor cells had large hyperchromatic nuclei. Later, on histopathological section papillary pattern with stromal invasion was noted. The case was diagnosed as papillary serous cystadenocarcinoma of ovary on histopathology. (Figure 4)
Figure 4
Case of papillary serouscystadenocarcinoma ovary (a): Photomicrograph of cytospin smear (i): showing tumor cells in papillae and 3D clusters (H&E, 10x), (ii) showing 3D balls of tumor cells with highly pleomorphic hyperchromatic nuclei and vacuolated cytoplasm (H&E, 40x). (b) Photomicrograph of cell block (i) showing tumor cells arranged in papillae, cords and clusters (H&E, 10x), (ii): showing papillae with tumor cells having large hyperchromatic nuclei (H&E, 40x).
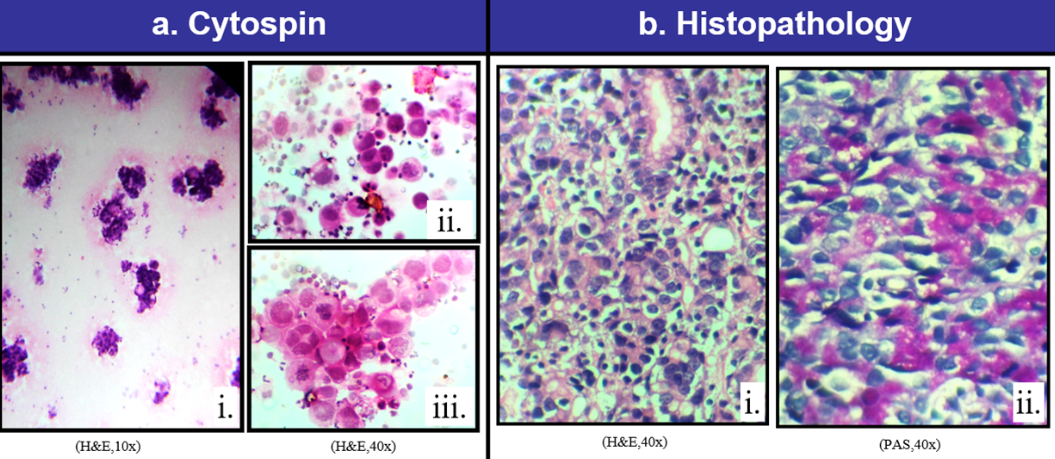
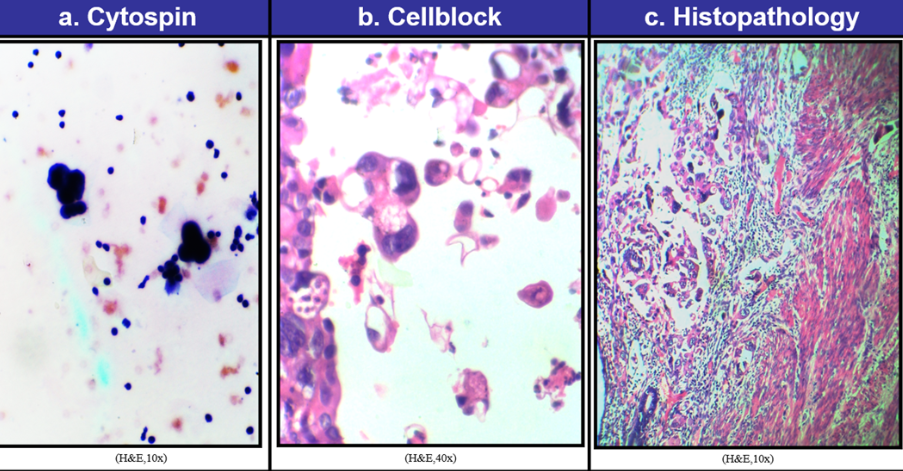
This study also had a case of gastric adenocarcinoma where the cytospin smear showed tumor cells in tight clusters with few signet ring cells. The cells were highly pleomorphic with hyperchromatic nuclei. Few mitotic figures were seen. Cellblock was also positive for tumour cells. Gastric biopsy of this case showed gastric mucosa with tumor cells in glandular pattern. Special stain was also performed and the tumour cells were PAS positive. (Figure 5)
Figure 5
Gastric adenocarcinoma, Case of gastric adenocarcinoma (a) Photomicrograph of cytospin smear (i) showing tumor cells in tight clusters with few signet ring cells (H&E,10x), (ii) showing highly pleomorphic tumor cells with hyperchromatic nuclei, (iii): showing many mitotic figures (H&E, 40x). (b): Photomicrograph of gastric biopsy (i) showing gastric mucosa with tumor cells in glandular pattern (H&E, 40x), (ii) showing Periodic acid-Schiff (PAS) positive tumor cells (PAS stain, 40x).
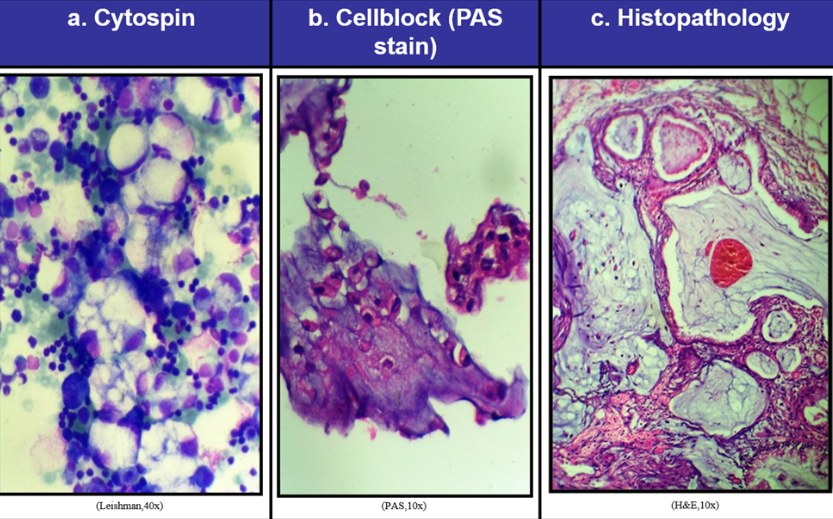
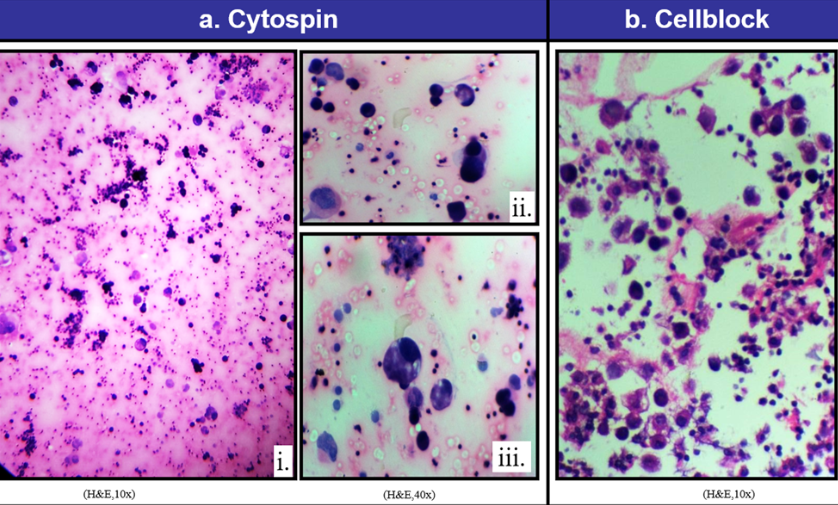
One case of adenocarcinoma colon, cytospin showed tumor cells in small clusters with many signet ring cells. PAS stain on cell block of the same showed signet ring cells with PAS positivity. Histopathological section of the omental nodule of this case showed tumor cells floating in large mucin pool. (Figure 6)
Figure 6
Case ofadenocarcinoma colon (a) Photomicrograph of cytospin smears showing tumor cells in small clusters with many signet ring cells (Leishman, 40x). (b): Cell block section showing signet ring cells with Periodic acid-Schiff positivity (PAS stain, 10x). (c): Photomicrograph of histopathological section of omental nodule in this case showing tumor cells floating in large mucin pool (H&E, 10x).
One case of adenocarcinoma rectum, cytospin showed tumor cells in cohesive clusters, 3D cluster with signet ring cells. Cellblock of the same showed tumor cells in glandular pattern and small clusters. (Figure 7)
Figure 7
Case of adenocarcinoma rectum; (a): Photomicrograph of cystospin smear; (i): showing tumor cells in cohesive clusters (H&E, 10x); (ii): showing 3D cluster of tumor cell with signet ring cells (H&E, 40x); (b): Photomicrograph of cell block section showing tumor cells in glandular pattern and small clusters (H&E, 10x).
One case of adenocarcinoma endometrium, cytospin showed tumor cells in small tight clusters forming 3D balls. Cellblock of the same showed tumor cells in small clusters and singles. Tumor cells had large pleomorphic hyperchromatic nuclei. It was diagnosed as diffuse high-grade adenocarcinoma of endometrium. (Figure 8)
Figure 8
Case of adenocarcinoma endometrium (a) Photomicrograph of cytospin smears showing tumor cells in small tight clusters forming 3Dballs (H&E, 10x). (b) Photomicrograph of cell block showing tumor cells in small clusters and singles. Tumor cells have large pleomorphic hyperchromatic nuclei (H&E, 40x). (c) Photomicrograph of histopathological section of endomyometrium showing diffuse high grade adenocarcinoma of endometrium (H&E, 10x).
One case of bronchogenic carcinoma, cytospin showed tumor cells in small clusters and singles. Cellblock showed tumor cells in small clusters and in singles with hyperchromatic large nuclei. (Figure 9)
Figure 9
Case of bronchogenic carcinoma (a): Photomicrography of cytospin smear (i): Showing tumor cells in small cluster and singles (H&E, 10X), (ii) and (iii): Showing highly pleomorphic tumor cells with large hyperchromatic nuclei (H&E, 40X). (b): Photomicrography of cells block section showing tumor cells in singles with hyperchromatic large nuclei (H&E, 10X).
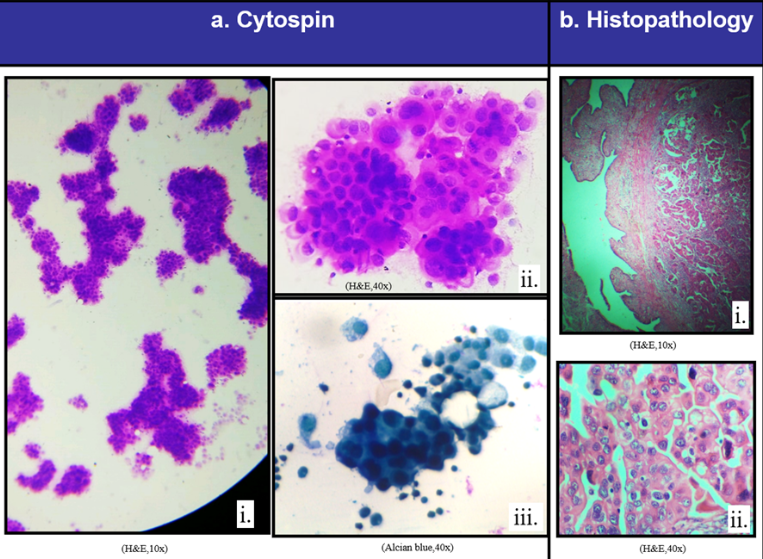
There was one interesting case where cytospin smear showed tumor cells in tight clusters, trabeculae and singles. Special stain performed on cytospin smear showed Alcian blue positive clusters and small sheets of tumor cells. Cellblock also showed tumour cells. Later, histopathological section of fallopian tube showed well differentiated adenocarcinoma. This case was diagnosed as synchronous high grade serous tumor of peritoneum and well differentiated adenocarcinoma of fallopian tube on histopathology. (Figure 10)
Figure 10
Case of synchronous high grade serous tumor of peritoneum and well differentiated adenocarcinoma of fallopian tube. (a) Photomicrograph of cytospin smear (@ showing tumor cells in tight clusters, trabeculae and singles (H&E, 10x).. (i) showing large tumor cells with pleomorphic nuclei (H&E, 40x), (iii) showing clusters and small sheets of tumor cells (Alcian blue, 40x). (b) PhotomicrogrCase of synchronous high grade serous tumor of peritoneum and well differentiated adenocarcinoma of fallopian tube. (a) Photomicrograph of cytospin smear @ showing tumor cells in tight clusters, trabeculae and singles (H&E, 10x).
This study showed sensitivity 96%, specificity 100%, positive predictive value of 100%, negative predictive value 96.4% and diagnostic accuracy 98% in detecting malignancy by cytological test. Cellular yield was 3.85% more by cellblock method when compared to cytospin smears. Statistical comparison with results from other studies are shown in Table 5, Table 6.
The presence of malignant cells in ascitic fluid and intraoperative peritoneal wash samples is a diagnostic challenge. Positive cytology in ascites almost always obviates explorative surgery. It is important for staging, prognosis and management of patients with malignancies. Ascites with positive cells almost always indicates metastasis and is associated with poorer prognosis.6 Many times diagnosis can be made on either cytospin or cellblock alone but using both the techniques on the same sample leads to more accurate diagnosis.2
Conclusion
Cytospin smears are no doubt a good method for cytodiagnosis, but cellblock can give additional information complimenting the diagnosis. Cellblock is a simple, rapid and inexpensive method. When used in conjunction with cytospin, cellblock can help in establishing accurate diagnosis by picking up the malignant cells. It can bridge the gap between cytology and histology. Thus, the combination of cytospin and cellblock helps in either confirming or disapproving malignancy.



