Introduction
Endometrial carcinoma (EC) is the 6th most commonly diagnosed cancer in women worldwide1 and the third most common gynaecological malignancy in South-Eastern Asia following cervical and ovarian carcinomas. 2 The most of the patients have a favourable 5-year relative survival rate if diagnosed at an early stage. 3 The overall 5-year survival rate is approximately 96%. 3 The disease is rare before 40 years age group and 80 % of the patients are in postmenopausal age at the time of diagnosis. 4 Majority of the carcinomas occurs sporadic with only 5–10% having a hereditary basis. 5 The major risk factors relate to hormonal stimulation of the endometrium in conditions like unopposed Oestrogen therapy, polycystic ovarian disease and oestrogen-producing tumours. 5 Obesity is observed in 50% of patients with endometrial carcinoma, and the risk is linked to disturbances in hormone metabolism related to obesity.6 The other risk factors include nulliparity, diabetes, hypertension and breast cancer patients treated with tamoxifen therapy (six- to eight-fold increased risk). 6
Endometrial hyperplasia is diagnosed with the presence of proliferating endometrial glands resulting in increase in gland-to-stroma ratio. 7 Endometrial hyperplasia is a recognized precursor lesion of the most common type of endometrial cancer (endometrioid) and its timely detection offers an opportunity for prevention of endometrial cancer. 1 However the rate of progression depends on factors such as the degree of architectural abnormality and the presence or absence of nuclear atypia. 8 Endometrial hyperplasia is seen most frequently in menopause or postmenopausal women, when there are anovulatory cycles. 9
The endometrium shows tightly controlled hormone-dependent variation during menstrual cycle and when this tightly controlled system is disturbed it may lead to series of changes which may initiate and promote the progression of endometrial tissue toward malignant phenotype. 10 These changes can be further divided into distinct steps involving activation of oncogenes or other proteins involved in tumor invasion and progression like self-sufficiency in growth signals, insensitivity to growth inhibition, evasion of apoptosis, angiogenesis, invasion and metastasis involving genetic alteration/activation of various oncogenes/other proteins. 5, 10 Oncogenes are usually present in inactive state, and their activation stimulates the process of cell division. Only few oncogenes are known to be altered in endometrial cancer. Amplification and increased expression of oncogene HER-2/neu is observed in 10% - 40% of endometrial carcinomas and its expression correlates with a poor prognosis and more aggressive tumour behaviour. 11
Her-2/neu is an oncogene located on the chromosome 17; encoding type 1 tyrosine kinase growth factor receptor. 12 Her-2/neu (c-erbB-2) gene expression plays an important role in coordinating the endometrial growth factor receptor signaling network. 10 When Her2/neu gene is expressed normally, it leads to the combination of a few copies of Her-2/neu heterodimers and the Her-2/neu-mediated signalling is weak resulting in a normal cell growth. 10, 13 But Her-2/neu Gene amplification results in 50-100 genes per cell leading to the expression of more than 2,000,000 Her-2/neu proteins per cell in the tissue, instead of the 20,000-50,000 Her-2/neu proteins per cell, leading to increase tyrosine kinase activity which in turn increases mitogenic cell signalling and increase cell proliferation activity and shows anti-apoptotic and neo-angiogenic effects. 14, 15 Her-2/neu oncogene amplification is seen in many human cancers like breast cancer, pancreatic cancer and ovarian cancers and it provides an attractive therapeutic target. 16
The development of Her-2-targeted therapies has revolutionized the treatment of HER2-positive breast cancer and has significantly improved their outcomes.17 A humanized monoclonal antibody directed against the extracellular domain of the Her-2 receptor is found to have a significant therapeutic effect in patients with Her-2/neu positive carcinomas as it prevents ligand-independent Her-2 signaling, down regulates Her-2/neu expression and diminishes more active p95–Her-2 form of Her-2. 18 Targeting Her-2/neu may be beneficial for a selected group of patient with endometrial carcinoma showing Her-2/neu overexpression. The present study is aimed to evaluate Her-2/neu protein overexpression in endometrial hyperplasia and carcinoma, its pattern of expression and correlation with histological type, and grade of tumour and clinical stage wherever possible.
Materials and Methods
Materials
The present study was conducted in the Department of Pathology, in a Tertiary Cancer Hospital in Hyderabad, retrospectively from January 2010 to June 2012.
Immuno-histochemical evaluation of a total 62 cases was conducted who were confirmed to have Endometrial hyperplasia (20 cases) and Endometrial Carcinoma (42 cases) and were obtain from endometrial curettings and hysterectomy specimens which were sent to the Department of pathology, MNJ Cancer Hospital and Research Institute, Hyderabad. The haematoxylin & eosin (H&E) stained slides of the cases were retrieved & screened for confirmation of diagnosis followed by selection of the appropriate paraffin blocks
Endometrial Carcinoma Tumor staging was performed according to the International Federation of Gynaecology Obstetrics (FIGO) staging revised in 2009 and TNM staging system. Demographic and clinical information like age at time of diagnosis, clinical presentation and parity was obtained and recorded.
Methods
Formalin-fixed, paraffin embedded tissue blocks of each of 62 cases were obtained and all hematoxylin & eosin-stained sections were reviewed, the quality of the material was checked, and the best sections from each specimen were selected. All microscopic slides were reviewed to confirm the pathological diagnosis and grading was done according to the International Federation of Gynaecology and Obstetrics (FIGO) grading system. Tumour staging was performed according to the FIGO classification and TNM staging system. Patient's medical records and clinic-pathologic characteristics were reviewed. 3𝜇m sections were taken on positively charged slides for IHC with HER-2/Neu. IHC was performed for HER-2/Neu using standard IHC protocol (DAKO). The Polyexcel HRP (non-biotin, micro-polymer based) DAB Detection system was used with adequate positive and negative controls.
Interpretation of IHC
Estimation of HER-2/Neu expression was evaluated under light microscope and uniform criteria were used according to College of American Pathologists (CAP)guidelines and criteria used in Badr E. H., et al study.10 Brown stain of the cytoplasmic membrane was considered positive for IHC Staining.
The intensity of HER-2/Neu staining was scored as:
In present study, Scores of 0 or 1+ was considered tumour negative for Her2/neu expression and specimens with 2+or 3+ staining were considered positive for HER-2/Neu antibody overexpression.
Statistical analysis
The data was entered and analyzed in SPSS. Frequencies and percentages of all the variables were computed. The chi-square test (X2) was used to evaluate the relation between histopathological parameters and immunohistochemical markers. The results were considered statistically significant if the P value was < 0.05
Results
Clinic-pathological characteristic of patients
Clinical presentation
A total 62 (20- hyperplasia & 42- Endometrial carcinoma) cases were included in the current study. The mean age was 50.56 ± 9.95 years, where 6 cases of simple hyperplasia were between age group 35 – 40 years and 4 cases were aged 41-50 years. 5 cases of complex hyperplasia were aged between 35- 40 years and 5 cases between 41-50 years.
While majority of patients with endometrial carcinoma (17 cases) were aged between 51-60 years, 13 cases were between 41- 50 years, 9 cases are between 61-70 years and 2 cases were above 70 years. (Table 1)
Table 1
Age wise distribution
In the present study, most of patients of simple hyperplasia presented with menorrhagia (8 patients), and only 2 patients with polymenorrhea. Majority of patients with Complex hyperplasia presented menorrhagia (7 patients), followed by post-menopausal bleeding (3 patients). In endometrial carcinoma 35 patients (83.33%) presented with postmenopausal bleeding followed by 7 patients (16.6%) with menorrhagia. Regarding parity of patients, majority of patients with endometrial carcinoma were in Parity 2 (20 patients) followed by Parity 1 (10 patients).
Type and Grade wise distribution of Endometrial Carcinoma
All the carcinomas were graded from I- III according to International Federation of Gynecology and Obstetrics (FIGO) grading system based on the degree of glandular differentiation. 17 cases (40.47%) were in Grade I, 10 cases (23.80%) were in Grade II and 15 cases (35.71%) were in Grade III. Among 42 cases of endometrial carcinoma, 38 cases (90.47%) were of Endometrioid adenocarcinoma (type 1) and 4 cases (9.52%) are of serous adenocarcinoma (type 2).Table 2
Endometrial Carcinoma staging
The tumour was staged according to TNM staging system based on pathology of primary tumour, lympho -vascular invasion and lymph node assessment and showed 17 cases of Stage I (Tumour confined to the corpus uteri only) of which 4 cases (9.52%) were Stage Ia, 10 cases (23.8%) of Stage Ib and 3 cases (7.14%) of Stage Ic. Followed by 9 cases of Stage II (Tumour invades cervix) of which 4 cases (9.52%) showed Endocervical glandular involvement only (Stage IIa) and 5 cases (11.9%) showed Cervical stromal invasion (Stage IIb).
16 cases were of Stage III (Local and/or regional spread of tumour) of which 13 cases (30.95%) showed Metastases to pelvic and / or para-aotic lymph nodes (Stage IIIc),whereas in 2 cases (4.76%) Tumour invasion into the B/L ovaries was seen and only in single case (2.38%) Vaginal involvement was seen. Table 3
Immunohistochemical analysis of HER-2/neu expression
All the 62 cases were subjected to Immunohistochemical staining with Her-2 antibody. The intensity of the staining was recorded and graded according to the standard protocol.
Her-2/neu expression analysis of endometrial hyperplasia showed total 9 cases (45%) showing positive Her-2/neu expression (+2 score) of which 3 cases were of simple hyperplasia and 6 cases were of complex hyperplasia. While 11 cases (55%) showing negative for Her-2/neu expression (0, +1 score).
Her-2 Immunoexpression analysis in Endometrial carcinoma showed, 23 (54.76%) of the cases showed moderate to strong complete membrane staining in more than 10% of the tumour cells (3+). 16 (38.09%) cases showed weak incomplete membranous staining or complete membranous staining in less than 10% of the tumour cells(1+) and only 03(7.14%) cases showed no membrane staining for HER-2/neu expression. The results are depicted in Table 4 .
Table 4
HER-2 Immunoexpression in Endometrial carcinoma
|
Diagnosis |
HER-2/neu expression assessment |
||
|
Endometrial carcinoma |
Absent (%) |
+1 (%) |
+2 & +3 (%) |
|
03 (7.14%) |
16 (38.09%) |
23 (54.76%) |
|
Based on the histological type of tumour, all the 4 cases of Serous Adenocarcinoma (type 2) showed positive HER-2/neu expression and 19 out of 38 of cases of Endometrioid Adenocarcinoma showed positive HER-2/neu expression.Table 5
Correlation between histopathological variables and Her-2/neu overexpression
In the present study, Patients with stag I-II disease were compared to those with stage III-IV regarding Her-2/neu expression. Statistically significant relation was reported between Her-2/neu expression and FIGO stage where 16 (94.12%) of patients with stage III-IV expressed positive Her-2/neu while only 07 (28%) of patients in stage I-II demonstrated positive Her-2/neu expression. (p <0.05) According to grade of differentiation, 14 cases with High grade (Endometrioid Grade-3 and serous Adenocarcinoma) showed positive Her-2/neu expression while 09 (33.33%) cases with Low to intermediate grade (Endometrioid Grade-1 and Grade-2) expressed positive Her-2/neu expression, the difference was significant (P <0.05).
Correlation between Her-2/neu expression and lymph node involvement demonstrated significantly higher rates (92.31%) of Her-2/neu expression in patients with lymph node metastases as compared to patients without lymph node metastases (37.93%) (p<0.05). Significant correlation was also reported in myometrial invasion, strong positive Her-2/neu expression was reported in 14 (73.68%) cases with ≥50% myometrial invasion while 09 (39.13%) with <50% myometrial invasion showed positive Her-2/neu expression (P <0.05). Significant correlation (P<0.05) was also reported in cervical invasion, with 17 (77.27%) cases with cervical invasion showing strong positive Her-2/neu expression and 6 (30%) case without cervical invasion showing positive Her-2/neu expression. Table 6
Table 6
Correlation between histopathological variables and Her-2/neu overexpression by IHC in Endometrial carcinoma
Figure 1
A: H&E endometrial glands with complex hyperplasia without atypia (10X); B: HER-2/neu immunoexpression in complex hyperplasia without atypia (40X)
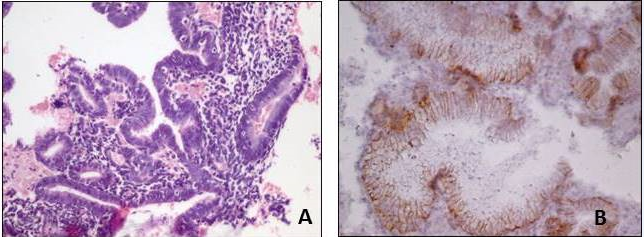
Figure 2
A: H&E endometrial glands with complex hyperplasia with Atypia (10X); B: HER-2/neu immunoexpression in complex hyperplasia with Atypia (10X)
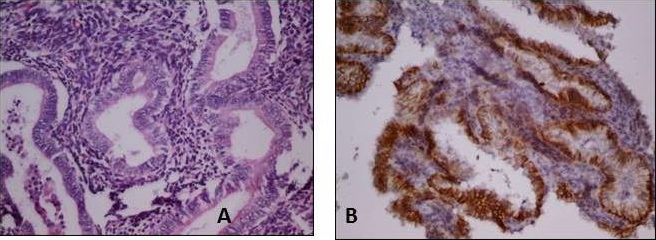
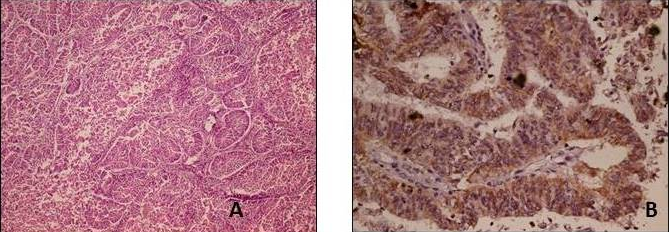
Figure 3
A: H&E Well differentiated Endometrioid Endometrial carcinoma (Scanner); B: HER-2/neu immunoexpression in Well differentiated Endometrioid Endometrial carcinoma (40X)
Discussion
Endometrial carcinoma is the commonly diagnosed gynecological malignancy in women and the incidence of endometrial cancer and associated mortality rates have increased in recent years. 19 Endometrial hyperplasia is a recognized precursor lesion of endometrial cancer and its timely detection offers an opportunity to prevent the development of endometrial cancer. Atypical endometrial hyperplasia shows features of cytological atypia of the glandular lining epithelium, stratification of epithelium, loss of polarity, increase in the nuclear/cytoplasmic ratio. 20
The pathogenesis of endometrial carcinoma and its transition from normal to neoplasm is complex and involve many molecular disturbances. Genetic abnormalities involve in development of endometrioid carcinoma are PTEN mutation, PIK3CA oncogene mutation, microsatellites instability (MSI), K-ras mutation, bet catenin inactivation, HER-2/neu overexpression. 11
Increase expression of the HER2/neu proto-oncogene, either due to gene amplification or due to transcriptional deregulation, is seen in many solid tumors like breast and ovarian carcinoma and associated with worse biological behavior and poor prognosis. 21 Smaller studies have suggested that Her-2/neu overexpression may be involved in the tumorigenesis of endometrial carcinoma as well. 21 Prognostic and therapeutic implication of Her-2/neu expression in endometrial carcinoma continue to evolve over recent years. In the literature, the reported rates of Her-2/neu overexpression and amplification in endometrial carcinoma varies from 17% to 80%. 10, 21, 22
The Her-2/neu overexpression has limited studies done with regard to its presence in cases of endometrial hyperplasia. The study done by Mariani et al 23 showed Her-2/neu overexpression was associated (borderline significance) with high-grade tumors and non-endometrioid histological subtypes. 23 Ioffe et al 24 observed that Her-2/neu expression was not present in atypical hyperplasia, whereas 30% of endometrial carcinomas did show Her-2/neu expression. In the present study, 20 patients with endometrial hyperplasia were evaluated for expression of Her-2/neu, 10 cases were of simple hyperplasia and 10 were of complex hyperplasia. Total of 9 cases (45%) of endometrial hyperplasia showed positive Her-2/neu expression (3 -simple hyperplasia and 6-complex hyperplasia), while 11 cases (55%) of endometrial hyperplasia were negative for HER-2/neu expression. This finding is in contrast with the study done by Eissa et al 25 study, 20% of endometrial hyperplasia showed HER-2/neu overexpression.
In the present study, analysis of Her-2/neu overexpression in endometrial carcinoma showed 54.76% of cases expressing a moderate to strong HER-2/neu staining in more than 10% of the tumour cells. This is comparable with Eldin et al 10 study which demonstrated 42.1% Her-2/neu overexpression in endometrial carcinoma cases. In Markova et al 11 study positive Her-2/neu overexpression was seen in 28.4% cases of endometrial carcinoma, whereas in the study done by Saffari et al26 52% endometrial cancers showed moderate or high HER-2/neu expression. Other studies that reported higher Her-2/neu expression are Cherchi et al.27 which showed 55.2% positivity and positive correlation with the grading, myometrial invasion and FIGO stage. In the study done by Yu et al 28 the positive expression rate of Her-2/neu in was 80.6%, significantly higher than that expressed in atypical hyperplasia endometrial tissue (2.8%).
In present study, a significant relationship was observed between Her-2/neu overexpression and FIGO stage of the tumor, lymph node metastases, myometrial invasion and cervical invasion indicating that Her-2/neu is related to most of the prognostic factors of Endometrial Carcinoma. Her-2/neu was strongly positive in 94.12% of patients with stage III-IV endometrioid adenocarcinoma while only 28% of patients in stage I-II demonstrated Her-2/neu expression. 93.33% of Grade 3 tumours showed Her-2/neu overexpression while only 29.63% of Grade 1 & 2 showed Her-2/neu overexpression. The present finding is in accordance with various studies like Eldin et al, 10 Cherchi et al, 27 Yu et al 28 where poorer the histological differentiation, higher the positive expression of C-erbB-2 was observed.
The present study demonstrated the positive expression of Her-2/neu in patients with lymph node metastasis (92.31%) or depth of myometrial invasion≥1/2 (73.68%) which was higher than those without lymph node metastasis or depth of myometrial invasion <1/2, indicating Her-2/neu expression increases with aggravation of lymph node metastasis and myometrial invasion. The present study also showed higher expression of Her-2/neu in patients with cervical invasion (77.27%). All above results suggest the statistical significant correlation (p < 0.05) between Her-2/neu overexpression and stage of the tumor, lymph node metastases, myometrial invasion and cervical invasion.
The finding of present study is comparable with Eldin et al 10 study, where 66.7% of Grade 3 tumors, 85% of advanced stage (stage III and IV) showed overexpression, 71% with lymph node metastasis and 70 % with >1/2 myometrial invasion showed strong HER-2/neu overexpression. Similarly, Cherchi et al, 27 Yu et al 28 also demonstrated a positive correlation between Her-2/neu expressions and grading, lymph node metastasis, myometrial invasion and FIGO stage.
Thus, HER-2/neu overexpression may be an important component in hormone-independent growth and proliferation of endometrium. HER-2/neu overexpression in complex endometrial hyperplasia may be a promising factor for the prediction of the progression to endometrial carcinoma. The findings in our study support the notion that Her-2/neu overexpression may be a major prognostic factor indicating a more malignant tumour phenotype and Her-2/neu Immunohistochemistry could be incorporated as a prognostic variable in patients with endometrial carcinoma. The patients with endometrial carcinoma showing strong Her-2/neu overexpression may potentially be benefited from Her-2-targeted Herceptin therapy improving their overall survival rate
Conclusion
In conclusion, present study provides evidence of Her-2/neu overexpression in a considerable proportion of the patients with Endometrial carcinoma, demonstrating statistically significant correlation between Her-2/neu expressions and FIGO stage, grading, lymph node metastasis ,myometrial invasion and cervical invasion, indicating Her-2/neu expression analysis could be an important prognostic factors of Endometrial carcinoma and suggesting the opportunity for the possible use of Her-2-targeted Herceptin therapy in selected patients improving their overall survival rate.



