- Visibility 38 Views
- Downloads 8 Downloads
- DOI 10.18231/j.achr.2021.057
-
CrossMark
- Citation
Importance of fine needle aspiration cytology in revealing the spectrum of axillary swelling: An experience with 30 cases
- Author Details:
-
Tina Rai *
-
G.S Rai
Introduction
Axilla is a triangular area between the lateral wall of thorax and the upper part of arm. It contains various nerves, blood vessels, lymph nodes & fatty tissue, so it is very important to know the anatomy of axilla. The diagnosis of the nature of the lesions could be easily made by Fine Needle Aspiration Cytology. FNAC has been emerging as an important diagnostic modality. It is a safe, cheap, less traumatic and easy diagnostic tool to differentiate between benign and malignant lesions. In experienced hands it helps to make an accurate diagnosis with less false negative results.[1], [2] Lymph nodes which are palpable and lymph node metastases from breast cancer are the most commonly encountered axillary masses However, various mesenchymal tissue elements are also present in the axilla such as fat, vessels and nerves which give rise to different lesions.[3] A combined approach of imaging techniques and FNAC improves the diagnostic accuracy of diagnosis and helps in avoiding unnecessary invasive procedures.[4], [5] This study was conducted to see the cytological spectrum of axillary lesions encountered in a tertiary care centre.
Aims and Objectives
To evaluate the role of Fine Needle Aspiration cytology in diagnosis of palpable axillary masses.
To document the spectrum of axillary swellings by FNAC.
Materials and Methods
Present study was carried out at the Department of Pathology. A total of 30 cases of axillary swelling which were referred for FNAC in the department of Pathology, over the period of 3 months (1stjuly to 1stOctober 2021) were retrospectively evaluated, all these patients who presented with superficial palpable swelling in the axilla were included. All the air dried smears that were stained with May Grunwald Giemsa and the alcohol fixed smears which were stained with Hematoxylin and Eosin and Papanicolaou stains were reviewed, Zheil-Neelsen stained slides of the cases were also reviewed.
FNAC smears along with relevant clinical information like age, gender, surgical information and radiological findings were retrieved from cytopathology records. The findings of FNA slides were reviewed, analysed and tabulated.
Results
Total 30 patients with palpable axillary masses came to OPD for FNA. FNAC was done and evaluated.
In the [Table 1] cases were distributed according to the Age. Maximum number of cases that is 10 were in the age group of 27 to 36 years followed by 7 cases in the age group of 16-26 years.
In Table no. 2, cases were distributed according to the Gender and the cytological diagnosis. There were 13 males and 17 females. On examining Papsmears, MGG staining and Ziehl Neelsen staining following diagnosis was made maximum number of cases that is 10 cases presented with chronic granulomatous lymphadenitis in which 8 were AFB positive, 8 cases presented with Reactive lymphadenitis In which 6 were females and 2 were males,1 case was of chronic nonspecific lymphadenitis, 5 cases presented with lipoma, 3 cases presented with Ductal carcinoma metastasis in the axilllary lymphnode which were confirmed on histopathology all cases were females, 2 cases presented with ectopic breast elements in the axillary lump, One unusual case of hydatid cyst who presenting with axillary swelling was diagnosed on AFB. The patient was 30 year male, on Pap smears and Giemsa only diagnosis of abscess could be made, but eventually on AFB the hooklets of the hydatid cyst were identified.
|
Age Group |
No. of cases (n=30) |
|
5-15 years |
6 |
|
16-26 years |
7 |
|
27-36 years |
10 |
|
37-47 years |
4 |
|
48-57 years |
2 |
|
58-67 years |
1 |
|
S.No. |
Cytological diagnosis |
No. of cases |
Males |
Females |
|
1. |
Chronic granulomatous lymphadenitis |
10 (33%) |
04 |
06 |
|
2. |
Reactive lymphadenitis |
8 (27%) |
2 |
6 |
|
3. |
Chronic nonspecific lymphadenitis |
1 (3%) |
1 |
0 |
|
4. |
Lipoma |
5 (16%) |
4 |
1 |
|
5. |
Ectopic breast tissue |
2 (7%) |
0 |
2 |
|
6. |
Ductal carcinoma breast metastases |
3 (1%) |
0 |
3 |
|
7. |
Hydatid cyst |
1 (3%) |
1 |
0 |
|
8. |
Total number of cases |
30 |
12 |
18 |
Cytology Findings
Chronic granulomatous lymphadenitis
Ten cases out of 30 were cytologically diagnosed as the cases of chronic granulomatous lymphadenitis showing well-formed granulomas, Langhans and foreign body giant cells in the necrotic background. 8 cases were AFB positive whereas 2 were AFB negative.
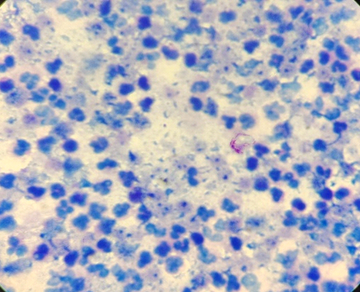
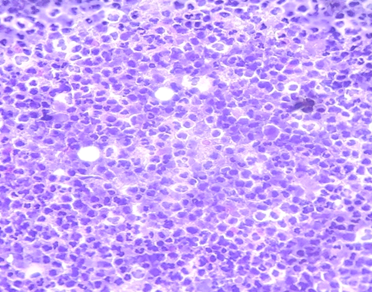
Reactive lymphadenitis
8 cases out of 30 were cytologically diagnosed as reactive lymphadenitis showing polymorphous population of centroblast., immmunoblast, centrocytes, lymphocytes, plasma cells and tingible body macrophages.
Chronic non - specific lymphadenitis
1 case out of 30 showed the picture of chronic nonspecific lymphadenitis comprising of mature lymphocytes.
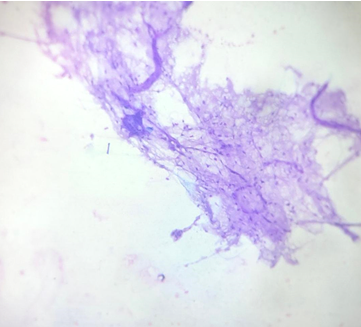
Lipoma
5 cases out of 30 were cytologically diagnosed as lipoma. The smears showed sheets of mature adipocytes and fibrous stromal fragments.
Ectopic breast
2 cases out of 30 showed ectopic breast elements. Smears showed tight cohesive monolayered sheets of benign duct epithelial cells, bipolar l nuclei in the fibromyxoid background.
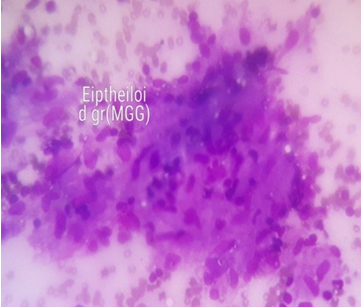
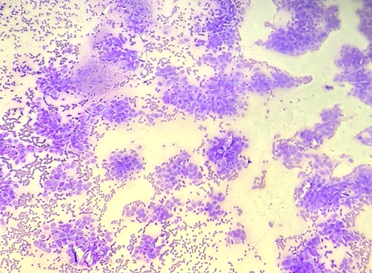
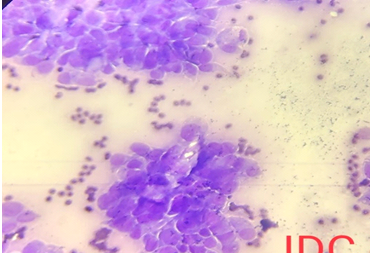
Metastatic infiltrating ductal carcinoma
This was seen in 3 out of 30 cases. The cytological features showed loose clusters and sheets of malignant duct epithelial cells, the cells were pleomophric having raise N:C ratio, moderate amount of cytoplasm, nuclear enlargement with irregular nuclear membrane, coarse clumped chromatin. The background showed haemorrhage and necrosis.
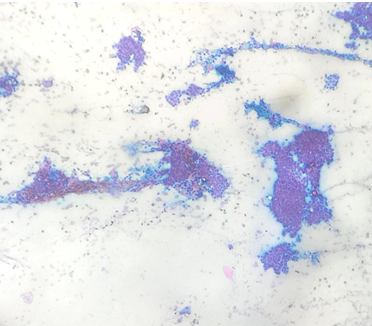
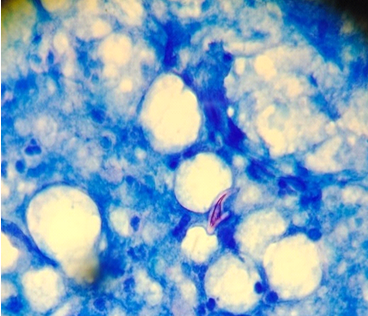
Hydatidcyst
One unusual case of hydatid cyst was seen in cytology: The MGG, H& E and PAP smears showed only necrosis but eventually on AFB the hooklets of the hydatid cyst were identified. The hooklets were semitransparent, refractile, and sickle shaped, with an inner semitransparent core of similar shape. Serological tests were performed for the confirmation which came out to be positive.
Discussion
Axilla is the pyramidal shaped space between the chest wall and the upper part of the arm. The various contents of axilla consists of axillary artery with its branches, axillary vein with its tributaries, brachial plexus with their branches, axillary lymphnodes, axillary fat and axillary tail of breast occasionally. Axillary lymph nodes are 20-30 in number these are anterior, posterior, lateral, central and the apical groups. The anterior group receives lymph from the major part of the breast, whereas the posterior group receives lymph from the axillary tail of the breast. The apical group receives lymph from the upper part of the breast. So, any disorder or any pathology which involves any of the above structures can lead to a mass in the axillary region. [6]
Axillary lesions are commonly encountered in lymphadenopathies, generally four cytomorphlogical patterns of lymphadenopathy were seen in our study like chronic granulomatous lymphadenitis, chronic nonspecific lymphadenits, reactive pattern and abscess formation. Apart, from the lymphnodes the other mesenchymal tissues present in the axillary region can also give rise to various lesions, the lesions may include accessory ectopic breast tissue, lipomas, hemangiomas, fat necrosis carcinoma of ectopic breast tissue rarely schwannoma, pilomatrixoma which has been discussed in certain studies and hydatid cyst as seen in our study are quite rare. FNAC is a simple, safe, rapid reliable and inexpensive method of establishing the diagnosis of lesions and masses at various sites and organs.[7], [8], [9], [10], [11], [12]
In our case chronic granulomatous lymphadenitis was the most common presentation of axillary swelling in which 8 were AFB positive. Granulomata are recognized cytologically as cohesive clusters of histiocytes of epithelioid type with or without associated multinucleated giant cells. a dirty necrotic background presence would suggest caseation and possibly tuberculosis[13] since granulomatous inflammmation in lymphnodes may be seen in various non-neoplastic as well as neoplstic conditions like Hodkins, NHL and metastaic carcinoma [14] Sen et al in their study have given the spectrum of cytomorphological pattern that can be seen in tubercular lymphadenitis, they stressed without AFB it’s difficult to rule out tuberculosis and in that cases other causes of granulomatous lymphadenitis should be taken into consideration.
In our case 8 were AFB positive whereas in our case 2 were negative. The absence of necrosis does not rule out tuberculosis, and ZN staining for AFB is imperative in all cases of granulomatous lymphadenitis. As was seen in two cases in our study, in such cases demonstration of AFB both in direct smears and culture from aspirate is necessary.
in our study 8 cases were reported as reactive lymphadenitis which showed polymorphous population of centroblast, centrocytes, immunoblast, plasma cells and tingible body macrophages, 6 were females and 2 were males, this spectrum is seen in infections as well as malignancy in our study it was second most common cause of axillary swelling followed by chronic granulomatous lymphadenitis.
Third common presentation of axillary swelling in our cases was lipoma, 4 males and 1 female, in which cytology showed sheets of mature adipocytes along with fibrous fragments Soram et al found in their study lipoma as the most common clinical presentation of axillary swellling.
Detection of breast metastasis in the axilllary lymphnode plays a very important role in deciding the treatment of the patient since it helps in the staging of the tumour. In our study 3 cases were having metastatic deposits of ductal carcinoma breast in the axillary lymph node, which was confirmed on the histopathology also. Alkuwari et al found the sensitivity of FNAC to detect metastases was 60%[15] whereas Hammon et al found sensitivity to be 100%. [16]
The prevelance of accessory breast in rare, t is about 0.6-6%. [17] Mammary ridge if it fails to involute it can give rise to ectopic bresast tissue. The mammary milk lines, which extend from groin to axillla, develop along the sides of the embryo during the 6th week of embryonic life.[18] So the accessory breast tissue can occur anywhere along the milkline, but its most frequent location is axilla, and at times the accessory breast tissue shows tenderness and swelling as monthly pre-menstural changes. In our study we found 2 such cases which were showing ectopic breast tissue in axilla.
One unusual case of hydatid cyst presented with axillary swelling was seen in our study. It’s causative agent is Ecchinococcus granulosus .Echinococcusgranulosus infection can develop in any organ or tissue, in humans hepatic and pulomonary localizations are more common.[19], [20] The presence of axillary swelling as a cystic swelling is quite rare .The cystic swelling could be categorized into parasitic conditions as well as non-parasitic conditions. Non parasitic conditions include ganglionic cyst, inclusion cysts and cystic hygromas and other group includes parasitic conditions and includes toxoplasmosis, coenurosis, filariasis and echinococossis.21] The patient was 36 year old male and farmer by occupation, he presented with non-painful cystic swelling of 6cm diameter in axilla gradually increasing in size since 15 days. His blood tests (CBC and blood chemistry) were unremarkable. His USG of axilla showed a large cystic swelling of 8 cm in the axillary region, his USG abdomen was unremarkable. cytology of the aspirate from the axilla revealed the presence of hooklets in Ziehl-Neelsen stain positive, in many studies it has been documented that hoooklets of Ecinnnococcusgranulosus are Ziehl-Neelsen and Fite-Faraco positive.[21], [22] Though cytology of hydatid cyst is not recommended in most of the studies due to fear of anaphylaxis and spread of infection, some studies have shown it to be relatively safe procedure for the diagnosis of hydatid cysts. In our case, this was an incidental finding on FNA as patient presented with subcutaneous axillary swelling. His compliment fixation test came out to be positive. So in endemic areas this differential diagnosis of cystic swelling in axilla should also be kept in mind.
Many rare tumours also arise in axilla. We saw a varied spectrum in the FNA of axillary swelling ranging from the most common granulomatous lymphadenitis to the rare hydatid cyst presenting as the axillary swelling.
Conclusion
FNAC is a safe, easy, cheap tool to differentiate between the benign and malignant lesions. It is the rapid and OPD procedure with minimal complications to the patients. If assisted by the radiological investigations its sensitivity further increases. This study highlights the spectrum of lesions that can present as the axillary swellings, which could be diagnosed on FNA which aids in the proper management of the case.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Source of Funding
None.
References
- I D Buley. Fine needle aspiration of lymphnodes. J Clin Pathol 1998. [Google Scholar] [Crossref]
- S Mitra, S Ray, Mitrapk. Fine needle aspiration cytology of supraclavicular lymphnodes : Our experience over a 3 year period. J Cytol 2011. [Google Scholar] [Crossref]
- E Y Kim, B K Han, J H Shin, S Y Hahn, S S Kang. Sonography of axillary masses :what should be considered other than the lymphnodes ?. J Ultrasound Med 2009. [Google Scholar]
- Y S Rajesh, S Ellenbogen, B Banerjee. Preoperative axillary ultrasound scan : its accuracy in assessing the axillary nodal status in carcinoma breast. 2002. [Google Scholar] [Crossref]
- M C Van Rijk, E E Deurioo, O E Nieweg, K G Gilhujis, JL Peterse, E J Rutgers. Ultrasonography and fine-needle aspiration cytology can spare breast cancer patients unnecessary sentinel lymphnode biopsy. Ann Surg Oncol 2006. [Google Scholar] [Crossref]
- A K Datta. Essentials of human anatomy. Superior and inferior Extremities. 9th Edn.. 2014. [Google Scholar]
- PV Heerde, J Miliauskas, A Field, SR Orell, GS Streett, D Whitaker. Lyphnodes. Fine Needle Aspiration Cytology. 4th Edn. 2005. [Google Scholar]
- Lioetf Koov, R A Spence. Fine needle aspiration cytology (FNAC) in diagnosis of granulomatous lymphadenitis. Ulster Med J 2006. [Google Scholar]
- R Sen, N Marwah, K B Gupta, S Marwah, R Arora, K Jain. Cytomorphological patterns in tuberculosis. Indian J Tuberc 1999. [Google Scholar]
- D K Das, J N Pant, K L Chachra, N S Murthy, L Satyanarayan, T C Thankamma. Tuberculosis lymphadenitis : correlation of cellular components and necrosis in lymph-node aspirate with A.F.B Positivity and bacillary count. Indian J Pathol Microbiol 1990. [Google Scholar]
- M Anirban, V Kumar, AK Abbas, JC Aster. Diseases of infancy and childhood. Robbins and Cotran Pathological Basis of Disease. 9th Edn. 2015. [Google Scholar]
- A K Kochhar, K B Patel, M Shah. Pttern of lymphadenopathy on fine needle aspiration cytology of superficial lymphnodes (A study of 150 cases). J Adv Res Biol Sci 2012. [Google Scholar]
- PV Heeerde, J Mliasuskas, A FIeld, SR Orell, GS Sterett, D Whitaker. lymph nodes. Fine Needle aspiration cytology. 4th Edn. 2005. [Google Scholar]
- V Koo, T F Lio, Raj Spence. Fine needle aspiration cytology ( FNAC ) in the diagnosis of granulomatous lymphadenitis. Ulster Med 2006. [Google Scholar]
- E Alkuwari, M Auger. Accuracy of fine-needle aspiration cytology of axillary lymph-nodes in breast cancer patients: a study of 115 cases with cyto-histologic correlation. Cancer 2008. [Google Scholar] [Crossref]
- M Hammon, P Dankerl, R Janka, DL Wachter, A Hartmann, R Schulz-Wendtland. Fine needle aspiration cytology of lymph nodes in breast cancer follow-up is a feasible alternative to watchful waiting and to histology. BMC Womens Health 2015. [Google Scholar] [Crossref]
- De Cholnokyt. Acessory breast tissue in axilla. N Y State J Med 1951. [Google Scholar]
- D D Alder, M Rebner, D R Pennes. Acessory breast tissue in axilla: Mammographic appearance. Radiology 1987. [Google Scholar] [Crossref]
- G S Guven, Simsekh, Cakirb, O Akhan, O Abbasoglu. A hydatid cyst presenting as an axillary mass. Am J Med 2004. [Google Scholar] [Crossref]
- J E Losanoff, B W Richman, J W Jones. Primary hydatid cyst of the axilla. Aust NZJ Surg 2004. [Google Scholar]
- P Brundelet. Acid-fast staining of hoooklets of Taeniaecchinococcus. Lancet 1973. [Google Scholar] [Crossref]
- K Ishak. Acid-Fast staining of hoooklets of Taeniaecchinococcus. Lancet 1973. [Google Scholar] [Crossref]
- Introduction
- Aims and Objectives
- Materials and Methods
- Results
- Cytology Findings
- Chronic granulomatous lymphadenitis
- Reactive lymphadenitis
- Chronic non - specific lymphadenitis
- Lipoma
- Ectopic breast
- Metastatic infiltrating ductal carcinoma
- Hydatidcyst
- Discussion
- Conclusion
- Conflicts of Interest
- Source of Funding
