Introduction
Nodular Fasciitis is an extremely rare benign reactive proliferative lesion of breast which was included as mesenchymal tumor of breast by the WHO classification in 2012. 1 Despite of its benign nature it resembles breast cancer in term of its clinical course and imaging findings. The mammographic appearance of breast fasciitis is that of a dense, irregular or spiculated nodule, with poorly defined margins. On FNAC and core biopsy, it is difficult to give specific conclusive diagnosis. Excisional biopsy is essential for confirmatory diagnosis and to avoid unnecessary surgical intervention.
Case Report
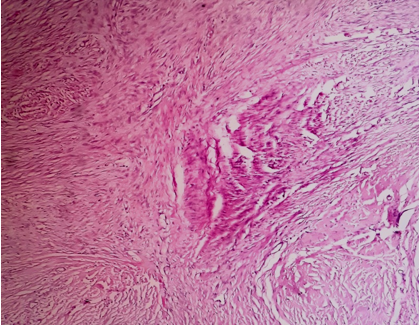
A 65 year female presented to oncosurgery unit for rapidly enlarging left breast lump in lower outer quadrant since 2 months. The lump was non-tender, firm and mobile. There was no nipple discharge. No axillary lymphadenopathy was detected. No history of any trauma or previous surgery of breast. There was no contributory family history. On sonomammography two masses, larger measuring 4 x 3.3 x 2.5cm, smaller measuring 2.0 x 1.6 x0.5cm were detected with hyperdensity and irregular margins and spiculations (Figure 1). The FNAC was done and reported as benign spindle cell lesion (Figure 2). The excisional biopsy of two masses were done.The larger mass measured 4 x 3.3 x 2.5cm, and smaller mass measured 2.0 x 1.6 x 0.5cm. On section showed a grey white, firm to hard ,glistening, irregular mass with irregular infiltrative margins in the surrounding brest parenchyma (Figure 3, Figure 4). On microscopic examination from multiple sections showed well circumscribed nodular lesions composed of neoplastic cells arranged in short fascicles, sheets and whorls. Neoplastic cells were elongated spindle cells having elongated or ovoid uniform nuclei with occasional prominent nucleoli and scant amount of cytoplasm. (Figure 5, Figure 6, Figure 7). The cellularity is variable from low to high. Mammary ducts and lobules are not present within the lesions. At the periphery of the lesion shows lymphoid aggregates. In areas tumor shows increased vascularity with extravasated erythrocytes. On histopathology reported as-Nodular Fasciitis of left breast mass. Immunohistochemistry showed reactivity to smooth muscle actin, negative for ER, PR, HER2/neu.
Figure 1
Sonomammography showed hyperdensity masses with irregular margin 4X3X2.5cm and 2x1.5x.0.6cm.
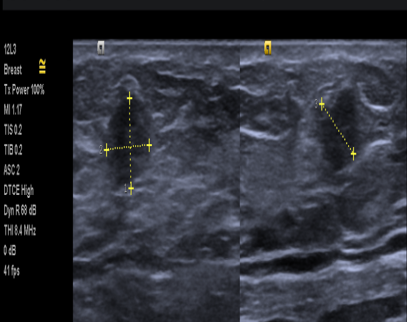
Figure 3
Wide excision of breast lump showing two masses larger m 4 x 3.3 x 2.5cm, and smaller m.2.0 x 1.6 x 0.5cm.
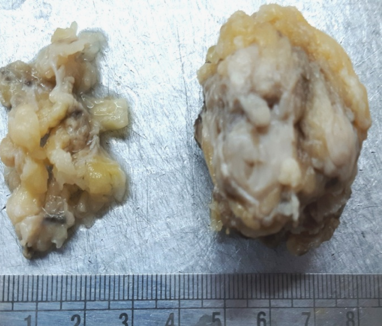
Figure 4
Gross specimen cut surface showing grey white, firm, mass lesion with irregular margins m 4 x 3.3 x 2.5cm.
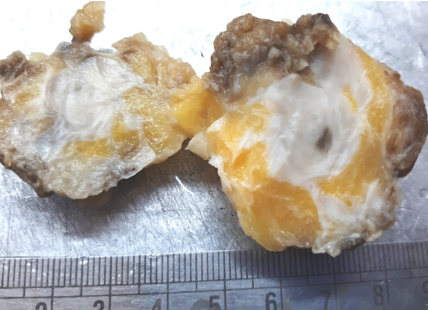
Figure 5
Photomicrograph showing circumscribed nodular lesions composed of neoplastic cells arranged in short fascicles, sheets and whorls.
Discussion
Nodular fasciitis was first described by Konwaler.2 Nodular fasciitis is a benign lesion due to proliferation of fibroblastic and myofibroblastic cells within subcutaneous tissue.3 It is commonly noted in soft tissue of upper limb and trunk. Nodular fasciitis in breast is extremely rare with approximately 150 cases reported. 4 The local injury to breast may trigger the fibroblastic proliferation and considered as one of the etiopathogenesis factor for nodular fasciitis breast. 5 The lesions of nodular fasciitis are similar to breast cancer on clinical and radiological imaging. 6 Clinically tumor grow rapidly. The age ranges from 17-84 year (average of 39 year). The size range from 0.5 to 5.5cm (average of 1.9cm.) In our case two nodular, irregular masses were detected. The lesions are firm to hard and irregular margins. The history of local trauma to breast is noted in 10-15% of cases. 7 On FNAC and core biopsy it is difficult to diagnose preoperatively. In our case reported as spindle cell neoplasm on FNAC. On USG and mammography most of the cases are reported as malignant. Mammography reveals an irregular, often spiculated lesion and ultrasonography detects an infiltrative mass without a capsule. The margins are often irregular. The perilesional invasion of the breast or fatty tissue is noted in many cases and mimic malignancy. The confirmatory diagnosis is only on histopathological examination which shows benign spindle cell proliferation of varying cellularity with irregular, infiltrating margins. The tumor is arranged in storiform pattern, short bundles. The individual cells are elongated having elongated nuclei with scant cytoplasm. Areas of atypia and cells with prominent nucleoli also noted. No pleomorphism and mitosis was noted. Background shows scanty myxoid material. For confirmation immunohistochemistry was done and which gives positivity for smooth muscle actin and vimentin and negative for ER,PR,HER2/neu. The differential like Fibromatosis, Myxoid sarcoma, Myofibroma, Phyllodes tumor etc. should be considered. In Fibromatosis large masses with usually dense collagenous stroma and linear fascicles of cells are noted.
In myxoid sarcoma/myxofibrosarcoma the tumors are usually deep soft locations and on microscopy shows alternating fibrous and myxoid areas with whorling tissues. The tumor composed of pleomorphic spindle cells in myxoid background. The high grade tumors are more cellular with atypical mitotic figures, hemorrhage, necrosis. 8 Myofibroma multifocal lesions having biphasic nodular pattern and frequent hemangiopericytoma -like vascular pattern are noted.
The diagnosis of nodular fasciitis is difficult and shoud be carefully differentiation from breast cancer is essential. On histopatholical exanimation nodular fasciitis is a spindle cell lesion marked by fibroblasts and myofibroblasts contained within a myxoid stroma. The nuclear atypia is absent.
The conservative management or excisional biopsy can be the treatment of choice for nodular fasciitis of breast. There is no malignant potential associated with nodular fasciitis, which makes prognosis excellent. In few clinically follow up cases spontaneous regression has been observed. It has been observed that the recurrence following surgical excision is rare. 9 rare cases of nodular fasciitis breast noted in male patients. 10, 11 We recommend breast conservative treatment provided that confirmation of nodular fasciitis is made clinically and histologically.
Conclusion
The diagnosis of nodular fasciitis can be mistaken as a breast malignancy due to its similarity with clinical, radiological, and histological features. We are presenting an extremely rare case of nodular fasciitis of the breast for its clinical radiological and histopathological presentation.




