Introduction
Endometrial pathology has become a predominate problem faced by women globally.1 Among the endometrial pathology, abnormal uterine bleeding is preponderate in developing countries.2 Abnormal uterine bleeding is an abnormal bleeding when there is an increase in the occurrence, in the duration and even in the quantity from the normal menstrual cycle.3 Abnormal uterine bleeding is still the universal complaint presented in obstetrics and gynaecology department. 4, 5 Abnormal uterine bleeding have a huge consequence on the women’s well being and financial burden on the universal health care system. 6, 7 Abnormal uterine bleeding which is claim to originate from organic causes and Dysfunctional Uterine Bleeding (DUB) is not due to organic causes. 8, 9 Abnormal uterine bleeding occur as menorrhagia, polymenorrhagia, metrorrhagia or menometrorrhagia. 10 Abnormal uterine bleeding are preferred to be treated medically11 and when the symptoms are non-responding to treatment. The pathology of endometrial tissues should be evaluated. There are many techniques for obtaining the endometrial tissue which are of minimal invasive such as endometrial curettage biopsies 12 ultrasonography endometrial biopsy, hysteroscopy endometrial biopsy, dilatation and curettage 13, 14 Among these techniques, endometrial curettage is safest and also shows an indistinguishable histopathology accuracy as of tissue samples from hysterectomy specimens in detection of endometrial pathology.15, 16 Our country despite of having advance medical technology, abnormal uterine bleeding is still the number one prevailing problem faced by our female population. In this study we wanted to analyse the percentage for endometrial pathology detected in women diagnosed with abnormal uterine bleeding.
Aim
To analysis the percentage for endometrial pathology by histopathological evaluation of endometrial curettage of women diagnosed with abnormal uterine bleeding in our tertiary care centre.
Materials and Methods
158 women patients who were diagnosed with abnormal uterine bleeding and their endometrial tissue sampling were histopathological evaluated for endometrial pathology. The study data were collected from February 2017 till January 2019 based on
Exclusion criteria
Pregnant women.
Systemic or non-pelvic causes of bleeding.
Inadequate samples.
Unfixed specimens.
Isolated cervical or vaginal pathology and leiomyoma.
The endometrial tissue samples were fixed, processed, embedded, staining and sectioning were done according histopathology laboratory protocol, and the slides were examined by a qualified MD Pathologist.
Results
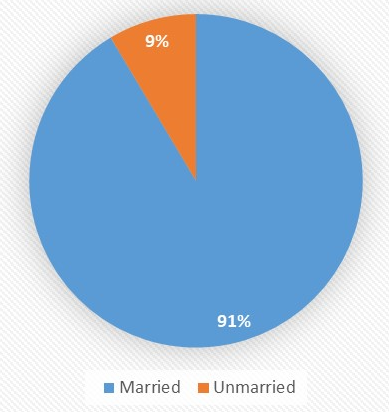
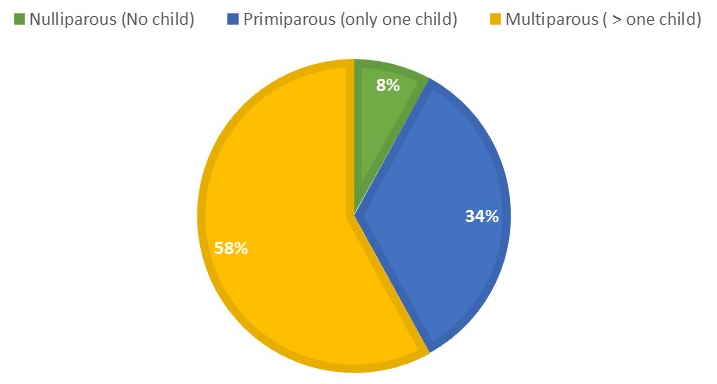
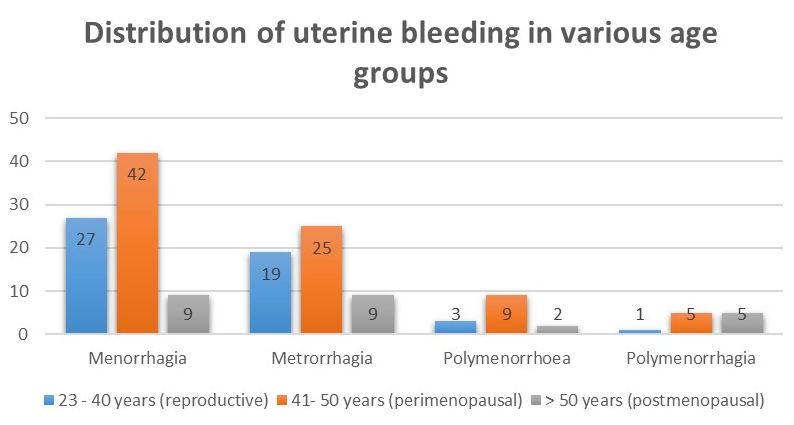
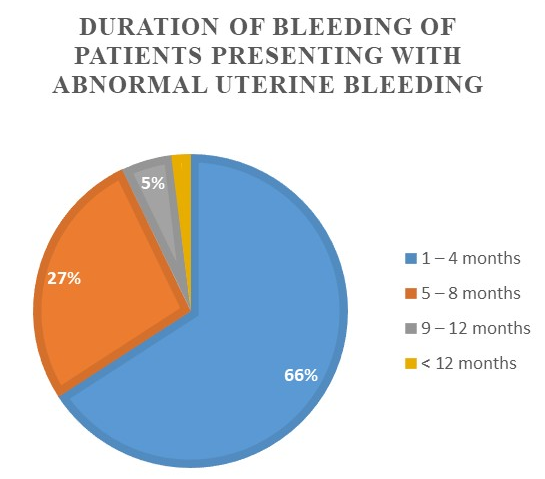
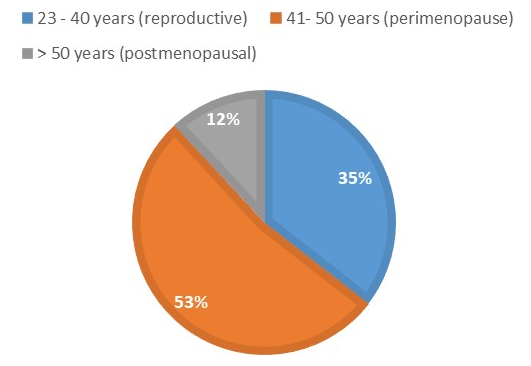
According to the inclusion criteria, the 152 women’s medical data, clinical information and endometrial histopathology finding were evaluated. 152 women patients who were diagnosed with abnormal uterine bleeding, their ages ranged from 23-78 years with a mean age of 43 years. Most of the patients were seen in the perimenopausal age group 52.63% followed by 35.53% in the reproductive age group and 11.84% in the postmenopausal age group. The 152 cases were distributed depending on marital status and the majority about 91.45 % were married and 8.55% were unmarried. Patients are distributed according to parity ranging from nulliparous to multiparous. Most of the women were multiparous about 58% and followed by primiparous 34%. About 8% women were nulliparous. Patients are distributed depending on the type of bleeding disorder, the commonest complaint was menorrhagia 51.32%. The perimenopausal age group were the most affected compared to the other 2 groups. Patients are distributed depending on the duration of bleeding, most of the patients about 65.29% presented a duration of bleeding between 1 – 4 months. The commonest endometrium histopathological finding observed in all the age groups was the proliferative phase which accounted for 38.82% and followed by the secretory phase in about 19.74% which were noted in the reproductive and perimenopausal age group. The disordered proliferative phase accounted for 14.47% which were noticed preponderance in the perimenopausal age group. Atrophic endometrium was noted in 5.92% which were present in the perimenopausal and postmenopausal age group. Endometrial polyp accounted for 5.26% noted in a reproductive and slight increase in perimenopausal age groups. Chronic endometritis accounted for 6.58% noted a slight increase in reproductive and perimenopausal age groups compared to the postmenopausal age group. Retained products of conception were 1.97% in the reproductive age group. Endometrial hyperplasia accounted for 5.92% noted in perimenopausal and postmenopausal age groups. Endometrial carcinoma accounted for 1.32% noted only in the postmenopausal age group.
Figure 1 152 patients presented with abnormal uterine bleeding and their ages ranged from 23-78 years with a mean age of 43 years. Most of the patients were seen in the perimenopausal age group 52.63% and followed by 35.53% in the reproductive age group and 11.84% in postmenopausal age group.
Figure 2 The 152 cases were distributed depending on marital status and majority about 91.45 % were married and 8.55% were unmarried.
Figure 3 Patients are distributed according to parity ranged from nulliparous to multiparous. Most of the women were multiparous about 58% and followed by primiparous 34%. About 8%women were nulliparous.
Figure 4 Patients are distributed depending on type of bleeding disorder, the commonest complaint was menorrhagia 51.32%. Perimenopausal age group were the most affected compared to the other 2 groups.
Figure 5 Patients are distributed depending on duration of bleeding, most of the patients about 65.29% presented duration of bleeding between 1 – 4 months.
Table 1
Shows the distribution of the histopathological evaluation in total cases.
Table 1 The commonest endometrium histopathological finding observed in all the age group was proliferative phase which accounted for 38.82% and followed by secretory phase in about 19.74% which were noted in reproductive and perimenopausal age group. Disordered proliferative phase accounted for 14.47% which were noticed preponderance in perimenopausal age group. Atrophic endometriumwas noted in 5.92% which were present in perimenopausal and postmenopausal age group. Endometrial polyp accounted for 5.26% noted in reproductive and slight increase in perimenopausal age groups. Chronic endometritis accounted for 6.58% noted a slight increase in reproductive and perimenopausal age groups compared to postmenopausal age group. Retained products of conception was 1.97% in reproductive age group. Endometrial hyperplasia accounted for 5.92% noted in perimenopausal and postmenopausal age groups. Endometrial carcinoma accounted for 1.32% noted only in postmenopausal age group.
Discussion
In our study, we observed 152 women patients were diagnosed with abnormal uterine bleeding, their ages ranged from 23-78 years with a mean age of 43 years. Most of them about 52.63 % were in their perimenopausal age [41-50 years], next 35.53% were in their reproductive age [23–40 years] and 11.84% were in their postmenopausal age [> 50 years] (Table 1). Perimenopausal was the commonest age group in our study and similar incidence were reported in other studies too. 14, 15, 16, 17
According to our study, 58% where multiparous similarly data were reported in other studies 18, 19 which is followed by 34% were primiparous and 8% were nulliparous were 2 of the nulliparous women were in the postmenopausal age group and their histopathological finding showed endometrial carcinoma according to literature, nulliparity is one of the risk factors for developing endometrial carcinoma. A similar finding was reported in 20% of nulliparous women in another study.20 The commonest complaint was menorrhagia in 51.32% among all the three age groups22 and 27.63% were from perimenopausal age group similar data were observed in other studies. 14, 15, 16, 17, 21, 18 The high incidence of menorrhagia were observed in the perimenopausal age group according to literature as menopause approaches there will be a decrease in the number of ovarian follicles and an increase in the resistance to gonadotrophic stimulation which produces low levels of oestrogen which reduce the normal endometrium growth leading to various patterns of abnormal bleeding.21
We observed 65.80% presented with excessive bleeding between the period of 1-4 months, among which 26.97% were from the perimenopausal age group which were a greater number of patients when compared to 2 other studies 38.06%14 and 30%.22 We observed the increase in the duration of excessive bleeding which increases with advancing of age.22, 23
We observed in our study the common histopathological finding of endometrial sampling was the proliferative phase which accounted for 38.82% of total cases, other similar studies showed variation from 28.36% to 53.91%. 16, 18, 24, 25, 26, 27, 28 Next followed by Secretory phase endometrium which accounts for 19.74% cases other studies showed variants of 16%, 25% and 30%. 25, 29, 30
Disordered proliferative endometrium is an amplification of the normal proliferative phase without any sign of an increase in the glands to stroma ratio as a cause of continuous oestrogen stimulation mostly seen in perimenopausal women. 21, 31 Our study 14.47% cases were reported with disordered proliferative endometrium and of which 15 cases were from the perimenopausal age group similar report were observed in other studies too. 32, 33 Atrophic endometrium is the commonest reason of bleeding in the postmenopausal stage. 34 The definite reason for atrophic endometrium is still unclear, the hypothesis may be due to prolonged absence of oestrogen leading to thinning and atrophic of the endometrium with variation in thinning of blood vessels and sensitivity to even minor injury and responsible for postmenopausal bleeding. 17, 30, 35 In our study atrophic endometrium was observed in 9 cases who were from both perimenopausal and postmenopausal age groups and accounted for 5.92% of total cases similar incidence was noted with variation from 1.1%-7% observed in other studies. 16, 17, 26, 27, 28, 30, 33, 34, 35, 36, 37 Endometrial polyps are formed due to lengthening of oestrogen stimulation the endometrium forms polyps 36 which according to studies the prevalence of endometrial polyps increase with advancing of age and lessens gradually after menopausal. The endometrial polyp in our study accounted for 5.26% of similar observations were seen in other studies. 35, 38 The endometrial hyperplasia in our study accounted for 5.92% which showed equal cases in the perimenopausal and postmenopausal age group. Endometrial hyperplasia is mostly diagnosed in perimenopausal 35, 39, 40 due to anovulatory cycles and to sustenance level of oestrogen which affects the endometrium and vascularisation causing irregular or prolonged bleeding.41 It is said to be a precursor of endometrial carcinoma. 39, 40 In other similar studies we observed variation from 5.79% -24.7%.15, 26, 27, 35, 36, 42 Chronic endometritis accounted for 5.79% of most of the cases seen in the reproductive age group. Plasma cells infiltration indicates chronic infection 43, 44, 45 caused by viral, chlamydial, or gonococcal which are usually observed after pregnancy, incomplete abortion and IUCD insertion,24, 27 similar data were observed in other studies.15, 26, 43
The retention of products of conception were about 2.48% from reproductive age group. Few studies have proved that abortion, pregnancy, and its related complication were most prevalent sources of abnormal uterine bleeding in the reproductive age group.18, 25, 41 In our study, we noted endometrial carcinoma accounted for 1.65% of cases, other similar studies have shown variation from 0.4% - 4.4%.17, 27, 36 Depending on the literature, endometrial carcinoma which is commonly seen in the postmenopausal age group17, 26, 40 like our study.
Conclusion
Histopathological evaluation is an onerous task for pathologists as not to miss any important findings and endometrial curettage tissue is the approved method for detecting any endometrial pathology. Our country despite being a developing country with advancements in medical technology, abnormal uterine bleeding is a prevailing problem. According to our analysis endometrial paraneoplastic lesions were detected from the reproductive age group. This study is done in an urban tertiary care centre, but we didn’t include the rural population, as 2 cases who were diagnosed with endometrial carcinoma in our study were from the postmenopausal age group, they were brought to our tertiary care centre for management by their relatives. All the rural primary health centres should be informed regarding the importance of endometrial tissue sampling and should be made a mandatory procedure for women who are affected with abnormal endometrial bleeding for early detecting and managing of low-risk women with abnormal uterine bleeding.