Introduction
Adenomatoid tumors are benign in nature with mesothelial origin.1, 2 They are commonly seen in male genital tract and account for 30% of all paratesticular tumors. They are the most common tumor of epididymis and spermatic cord in males.2, 3 In females, it is commonly seen in the myometrium and fallopian tubes. Adenomatoid tumors are uncommon in ovary and only few cases are reported till date.2, 4
Masson et al designated the term ‘benign mesothelioma of the genital tract’ in 1942, then Golden and Ash coined the term ‘adenomatoid tumor’ in 1945 to these benign, often incidental, and typically well-circumscribed neoplasms of mesothelial origin. 5
Similar to well differentiated papillary tumors, adenomatoid tumors are genetically defined by somatic missense mutation in TRAF7 gene. They present with intact nuclear expression of BAP1 and uniformly lack BAP1, CDNK2A and NF2 mutations or deletions that is characteristic of mesothelioms.
Case Presentation
A 62-year-old female presented to the gynecology clinic complaining of vague left-sided abdominal pain since one year that radiated to her back. She was postmenopausal from age of 47. There was a past surgical history of bilateral tubal ligation. A subsequent pelvic ultrasound was performed. The right ovary measured approximately 3.6 × 3 × 3.2 cm. In the right adnexal region dense acoustical shadowing was appreciated. The right ovary was nearly completely replaced by a heterogeneous solid mass. Serum tumor markers –alpha fetoprotein, beta‑human chorionic gonadotropin, and lactate dehydrogenase were within normal limits. The patient underwent total hysterectomy with bilateral oophorectomy.
Grossly, the specimen consisted of uterocervix with attached bilateral fallopian tubes and ovaries (Figure 1). On examination, uterocervix, bilateral fallopian tubes and left ovary was grossly normal. Right ovary was enlarged and smooth surface, cut section solid tan-white homogeneous are measuring a 3.6 × 3 × 3.2 cm.
Figure 1
Gross picture showinguterocervix with bilateral ovaries and fallopian tubes. Enlarged right ovary showing smooth external surface and solid tan-white homogeneous cut surface.

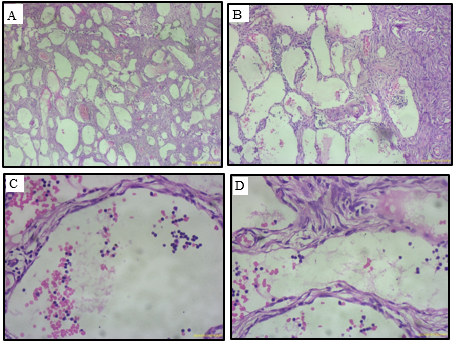
Microscopically, the ovarian solid nodule showed an unencapsulated, circumscribed tumor. The tumor was composed of spaces and clefts (Figure 2A and B) lined by low columnar, and flattened epithelial-like cells (Figure 2C and D), predominantly arranged in adenoid and glandular patterns. Some tumor cells exhibited marked vacuolation. Cytologic atypia and mitoses were absent.
Discussion
Adenomatoid tumors in ovarian and juxtaovarian sites are very rare. In females, these tumors are commonly reported in the age group of 23 to 79 years. Mean age being 54 year. They are small, asymptomatic tumors that completely replace the ovarian parenchyma and an incidental finding during ultrasonographic examination.
Adenomatoid tumors follow a benign course, their malignant transformation has not been reported. Surgical excision of the tumor is curative.
Adenomatoid tumors show a variety of morphological patterns including
Adenoid
Angiomatoid
Cystic
Canalicular
Glandular
Solid
Plexiform
Tubular. 6
The most common types are adenoid and angiomatoid. Cystic variant of adenomatoid tumor is the least common type and very rare.7 Adenomatoid tumors in genital tract exhibit an infiltrative pattern, which may lead to diagnostic difficulty.
The essential criteria include variably sized slit like tubular and cystic spaces that may have papillae with mesothelial lining. Immunohistochemistry of calretinin, WT1, D2-40, cytokeratin AE1/AE3 and CAM5.2. are positive.
Table 1
Comparison of studies ofadenomatoid tumors.
|
No. |
Author and citation |
Age-gender-side |
Greatest dimension |
Clinical findings |
Gross |
Histological patterns |
|
1. |
Sun Let al 1 |
58-F-R |
3x3x2cm |
Pain |
Solid and cystic |
Adenoid, solid, cystic. |
|
2. |
Shi M et al 2 |
44-F-R |
3.6x3x3.2cm |
Pain |
Solid |
Adenoid and glandular |
|
3. |
Vinaya SB 8 |
50-F-L |
4x3x3cm |
PV bleed, pain |
Solid |
Tubular and cystic |
Ovarian adenomatoid tumor could mimic malignancy, therefore it is important to identify these tumors and avoid over resection. There are a variety of tumors that can be considered for their differential diagnosis. These include lymphangioma, hemangioma, metastatic signet ring type carcinoma, epithelioid hemangioendothelioma, and yolk sac tumor.
Differential diagnosis of metastatic signet ring type carcinoma shows proliferation of signet rings ring cells with intracellular mucin that displaces nucleus to side.9 Hemangioma, on gross examination shows a small mass with red purple external surface and spongy, honey comb appearance filled with blood or serous fluid on cut surface. Microscopy shows lobules of capillary sized vascular channels, lined by single layer of flattened endothelial cells with lymphocyte infiltrate.10 Lymphangioma is mostly seen in children and microscopically shows thin walled capillaries, dilated lymphatic channels with intraluminal proteinaceous material and lymphocytes. Yolk sac tumors show structural similarity with adenomatoid tumors. Yolk sac tumors can be identified by the presence of schiller-duval bodies and remarkable cellular atypia.1
Conclusion
It is crucial to know this benign subtype of mesothelial tumor and diagnose these tumors in the frozen section to prevent more aggressive surgery.
Declaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.