Introduction
Collagenous gastritis is a rare and poorly understood condition characterized by the presence of a thickened subepithelial collagen layer in the gastric mucosa. This disorder shows a bimodal age distribution, affecting both pediatric patients and adults, but with different patterns of involvement. In children, the collagen deposition typically affects the gastric body or fundus, while in adults, it predominantly involves the antrum. Although the exact etiology remains unknown, patients often present with non-specific gastrointestinal symptoms. Here, we report a case of collagenous gastritis in a 50-year-old male who presented with recurrent vomiting, highlighting the challenges in diagnosis and management of this uncommon disease.
Case Report
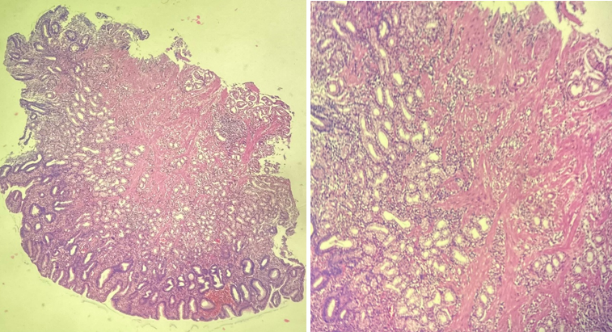
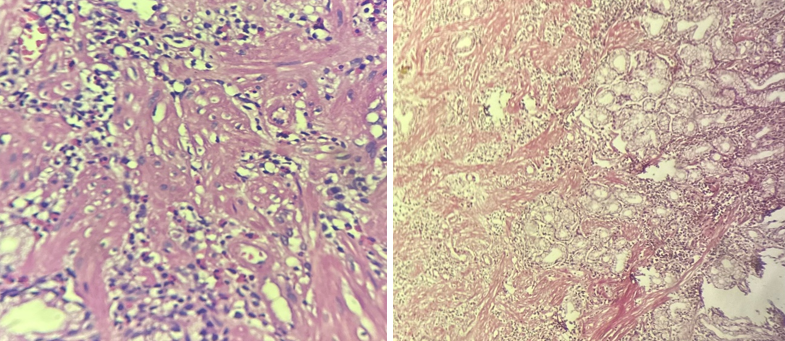
A 50 year old male patient came to medical gastroenterology department with complaints of vomiting. There is significant history of alcohol intaske.Endoscopy was done and multiple spots were identified in the stomach. Multiple biopsies were taken and send to our department for histopathologicalexamination.We received multiple grey white mucosal bits which were processed routinely and examined.
On microscopy mucosa was seen lined by columnar epithelium. Lamina propria showed extensive areas of collagenisation with fibrosis with entrapment of mucosal glands. Inflammatory cells predominantly lymphocytes, eosinophils were seen. Vangieson demonstrated collagen bands confirming the diagnosis of collagenising gastritis.
Discussion
Collagen gastritis is a very rare clinicopathological entity.1
Etiology of the disease was proposed to be due to primary vascular abnormality causing increased vascular permeability and collagen deposition.2
It covers under the broad category of collagenous gastroenteritis which includes collagenous gastritis and collagenous colitis. These are charecterised by mucosal subepithelial collagen deposition along with mucosal inflammatory infiltrate.3, 4, 5, 6 Paediatric patients presenting with upper GI symptoms with abdominal pain and anaemia where adults present with autoimmune proctitis and caeliac disease.7, 8 Upper endoscopy is recommended diagnostic modality.
More cases are needed to be documented to establish a standard therapeutic strategy.