- Visibility 49 Views
- Downloads 7 Downloads
- DOI 10.18231/j.achr.2024.042
-
CrossMark
- Citation
Concomitant benign serous cystadenoma with struma ovarii - An unusual combination of tumours from different origin, a case report and review of literature
Introduction
Struma ovarii is a rare ovarian tumour of germ cell origin which accounts for less than 5% of all ovarian neoplasms and is classified as monodermal teratoma. It can occur alone or in associated with other epithelial ovarian neoplasms. The coexistence of struma ovarii with serous cystadenoma is extremely uncommon with only 6 cases reported so far until 2017.[1], [2], [3] Struma ovarii has been reported to coexist with other ovarian tumours like mucinous cystadenoma, Brenner tumour, ovarian fibroma, thecoma, focal hilus cell hyperplasia, etc.[4] Herein, we report an extremely rare case of a 39-year-old woman who presented with an ovarian mass. Clinicoradiologically possibility of a right ovarian cyst with torsion was made. Histopathological examination revealed an unusual dual pathology – benign serous cystadenoma and struma ovarii. This case is reported to highlight the importance of extensive sampling and careful histopathological examination even in a grossly looking benign cystic lesion of the ovary. This case is presented due to its extreme rarity which can cause diagnostic dilemmas and to provide insight into rare entities and its prognostic significance.
Case History
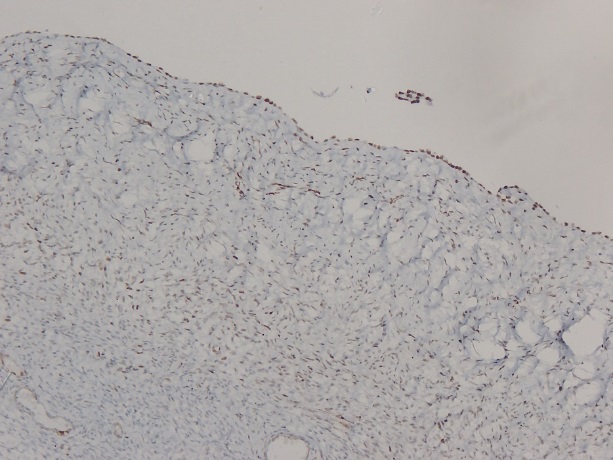
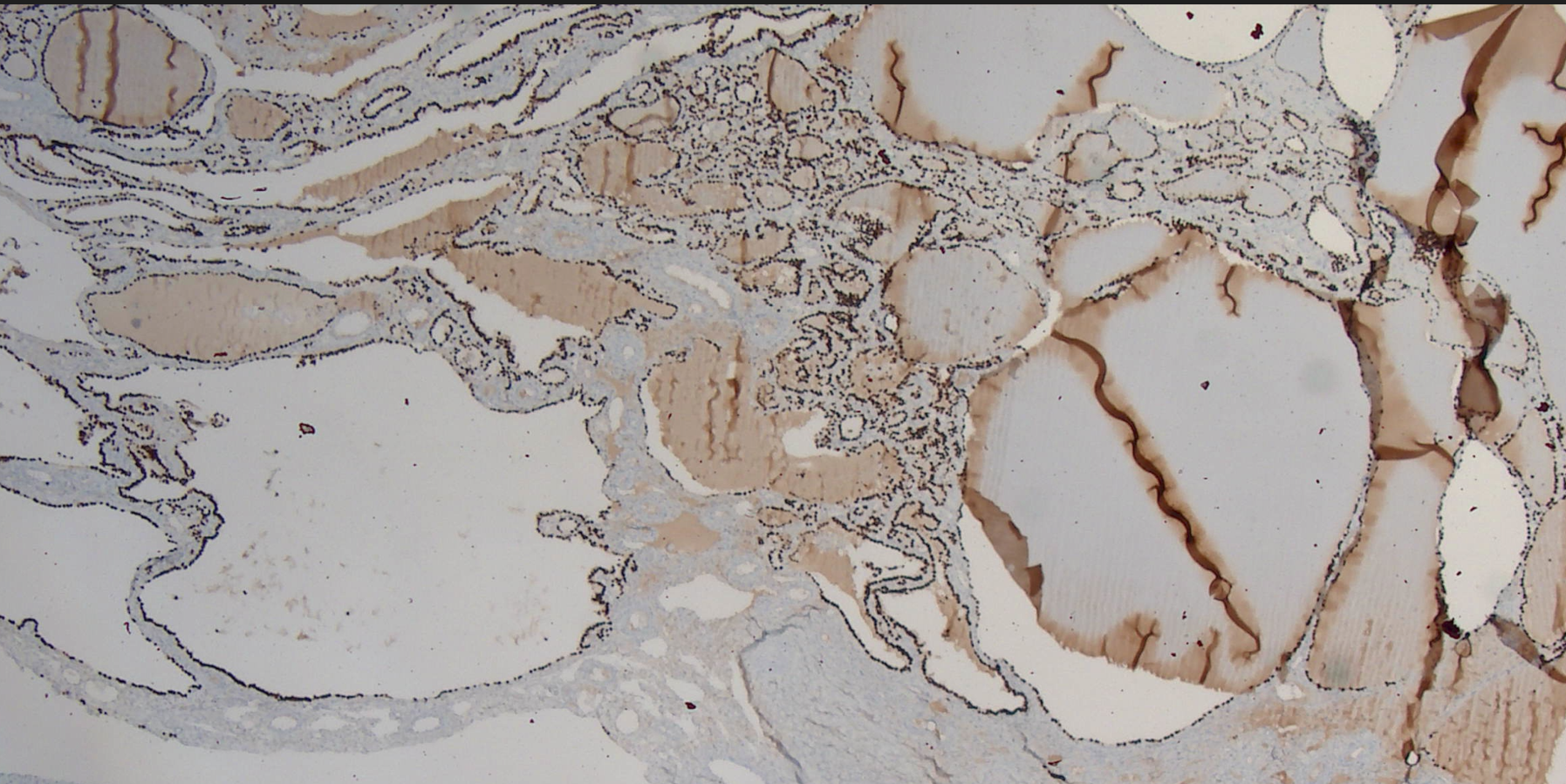
A 39 year old female, P2L2 (sterilisation done) presented with right sided abdominal pain on and off since 10 days. History of vomiting was present. Patient had regular menstrual cycles except for the past 1½ years during which her cycles were irregular. A clinical diagnosis of right ovarian cyst with torsion was made. There was history of laparascopic left ovarian cystectomy, which was done elsewhere 1½ years back, reports of which were not available with the patient. On examination, abdomen was soft and not distended. Ultrasound (USG) abdomen and pelvis showed a large cyst in the posterosuperior part of the uterus – right ovarian in origin, largest cyst of size 12.6x12x9cm with multiple thin internal septae. Laparascopic right ovarian cystectomy and detorsion was done under general anaesthesia. Intraoperatively, pneumoperitoneum was created, right ovarian cyst with torsion was visualized and detorsion was done. The cyst was ruptured iatrogenically during the intraoperative period. On gross examination, an already cut opened cyst measuring 7x5.5x2cm was obtained. The external surface of the cyst was smooth with focal areas of congestion. Further cutting open the cyst showed a uniloculated cyst with an average wall thickness of 0.1-0.2cm. The inner surface of the cyst appears smooth with focal brown areas. There are no solid areas or papillary excrescences identified. Histopathological examination showed fibrocollagenous cystwall lined by flattened epithelium and few strips of cystwall composed of varyingly sized follicles lined by cuboidal epithelium containing eosinophilic material resembling colloid amounting to ~1% of the total cystwall examined ([Figure 1], [Figure 2]). Based on the above histomorphology, a diagnosis of benign cyst - serous cystadenoma with focal areas showing follicles containing intraluminal eosinophilic secretions resembling thyroid parenchyma, no evidence of malignancy was made - Possibility of a Benign serous cystadenoma with co-existent cystic struma ovarii (though rare) needs to considered after evaluation by Immunohistochemistry for exact categorisation of follicles with intraluminal eosinophilic secretions. The cystwall was all embedded and no other germ cell derivatives were noticed histologically. On immunohistochemistry (IHC), the thyroid tissue was positive for CK7, TTF-1, PAX-8, CD56 and CK 19. The flattened epithelium was positive for CK7, PAX-8 and WT-1 ([Figure 3], [Figure 4]). Ki 67 was 4-5%. Postoperative period was uneventful and the patient was discharged in a stable condition.
![Fibrocollagenous cystwall focally lined by flattened epithelium (Right side) and colloid filled follicles of varying sizes lined by cuboidal epithelium (Left side) [H&E at 40x]](https://s3-us-west-2.amazonaws.com/typeset-prod-media-server/a5c573c6-a55e-4aa6-af67-fb9a2830e79dimage1.jpeg)
![Colloid filled follicles of varying sizes lined by cuboidal epithelium [H&E at 200x]](https://s3-us-west-2.amazonaws.com/typeset-prod-media-server/a5c573c6-a55e-4aa6-af67-fb9a2830e79dimage2.jpeg)
Discussion
Struma ovarii is a rare ovarian tumor which is defined by the presence of thyroid tissue comprising more than 50% of the total tissue examined. It was first described by Boettlin et al. in 1899.[5] Struma ovarii can occur as a part of a teratoma or rarely in co-existence with serous or mucinous cystadenomas. Struma ovarii accounts for ~1% of all ovarian tumors and 2-5% of ovarian teratomas.[6] Struma ovarii /monodermal teratoma is an ovarian neoplasm of germ cell origin which is composed predominantly of mature thyroid tissue. Cystic Struma ovarii is a variant of struma ovarii which is characterised by minimal thyroid tissue and cystic change thereby leading to diagnostic difficulties. As cystic struma ovarii shows minimal thyroid tissue, they can be missed if not sampled extensively. The co-existence of two tumors with different histogenesis in a neoplasm is rarely encountered. In the present case, serous cystadenoma of surface epithelial origin is seen in co-existence with Cystic struma ovarii which is of germ cell origin. Szyfelben et al proposed that the reported cases of struma ovarii associated with cystadenoma probably might represent an exclusively thyroid type cystic lesions.[7] Possibility of serous cystadenoma with coexistent struma ovarii could be due to the fact the serous cystadenoma could have been due to metaplasia of ovarian surface epithelium. Another possibility is that teratoma could have been from ovum evolved in a graffian follicle which failed to rupture and the epithelial component could be due to metaplasia of the lining epithelium.[8] Due to rarity of the lesion there is no clear hypothesis as to the reason for co-existence of the two lesions. This report highlights the importance of histopathological examination which is the gold standard in the diagnosis of Cystic struma ovarii with minimal thyroid tissue. The importance of identifying the struma ovarii component – thyroid tissue lies in the fact that various pathologies which occurs in thyroid gland can occur in the struma ovarii also. When the cause of hyperthyroidism is not obvious, struma ovarii could be a possible cause.
Conclusion
This case is reported to highlight the importance of extensive sampling and careful histopathological examination even in a grossly looking benign cystic lesion of the ovary. This case is presented due to its extreme rarity which can cause diagnostic dilemmas and to provide insight into rare entities and its prognostic significance. Any follicle or cystic structure with intraluminal eosinophilic secretion resembling colloid warrants thorough sampling and confirmation of the diagnosis by immunohistochemistry if required as to the presence or absence of a component of Struma ovarii and to confirm/exclude other components of teratoma including immature elements.
Sources of Funding
None.
Conflict of Interest
None.
References
- T Terada. Coexistence of struma ovarii and serous cystadenoma of the ovary. Int J Gynecol Pathol 2012. [Google Scholar]
- SP Kataria, A Batra, G Singh, E Boombak, R Sen, S Singh. Serous Cystadenoma Associated with Cystic Struma Ovarii: A Rare Entity. J Gynecol Surg 2014. [Google Scholar]
- Av R, GC Fernandes. A Rare Case Report Of Cystic Struma Ovarii With Co-Existing Serous Cystadenoma. J Postgrad Gynecol Obstet 2015. [Google Scholar]
- P Tang, S Soukkary, E Kahn. Mature cystic teratoma of the ovary associated with complete colonic wall and mucinous cystadenoma. Ann Clin Lab Sci 2003. [Google Scholar]
- SJ Kim, K Pak, HJ Lim, KH Yun, SJ Seong, TJ Kim. Clinical diversity of struma ovarii. Korean J Obstet Gynecol 2002. [Google Scholar]
- D Utsunomiya, S Shiraishi, K Kawanaka, F Lwakatare, S Tomiguchi, R Kido. Struma ovarii coexisting with mucinous cystadenoma detected by radioactive iodine. Clin Nuclear Med 2003. [Google Scholar]
- WM Szyfelbein, RH Young, RE Scully. Struma Ovarii Simulating Ovarian Tumors of Other Types A Report of 30 Cases. Am J Surg Pathol 1995. [Google Scholar]
- JK Mckenney, RA Soslow, TA Longacre. Ovarian mature teratomas with mucinous epithelial neoplasms: morphologic heterogeneity and association with pseudomyxoma peritonei. Am J Surg Pathol 2008. [Google Scholar]
