Introduction
Cutaneous leiomyosarcoma (cLMS) is a rare malignant mesenchymal tumour of the skin. This entity is also known as atypical smooth muscle tumour. It most commonly occurs in elderly Caucasian patients with peak incidence between fifth and seventh decades of life. A male predilection is noted with male to female ratio of 3:1 to 4:1.1 It comprises 2-3% of all cutaneous soft tissue sarcomas. The typical presentation of cLMS is as small (0.5-3cm) occasionally painful nodule over trunk and lower extremities. 2 cLMS are grouped into 03 clinicopathological categories each having different prognostic implications and risk of local recurrence and distant metastasis. 3 These include dermal lesions (limited to dermis), hypodermal lesion (involving subcutaneous tissue) and cutaneous metastasis of extracutaneous leiomyosarcoma. Deeper the lesion, worse is the prognosis. Dermal LMS arises from dermal arrector pili muscles, dartos muscle of skin or areolar muscles of breast whereas subcutaneous LMS arises from smooth muscle layer of vessel walls of arteries and veins. By virtue of its deeper location, subcutaneous LMS has a higher tendency of local recurrence (37%) and distant metastasis (21-62%) compared to dermal LMS (24% and 03-14% respectively). 4 Cutaneous metastasis of extracutaneous LMS has the worst overall prognosis. Rare association of cLMS with Birt-Hogg-Dube syndrome, Li Fraumenni syndrome and EBV infection in immunocompromised patients have been reported. 1, 5 Herein, we present interesting and rare case report of cLMS revealed by histopathological examination of circumcised prepuce in an elderly male who presented with phimosis.
Case Summary
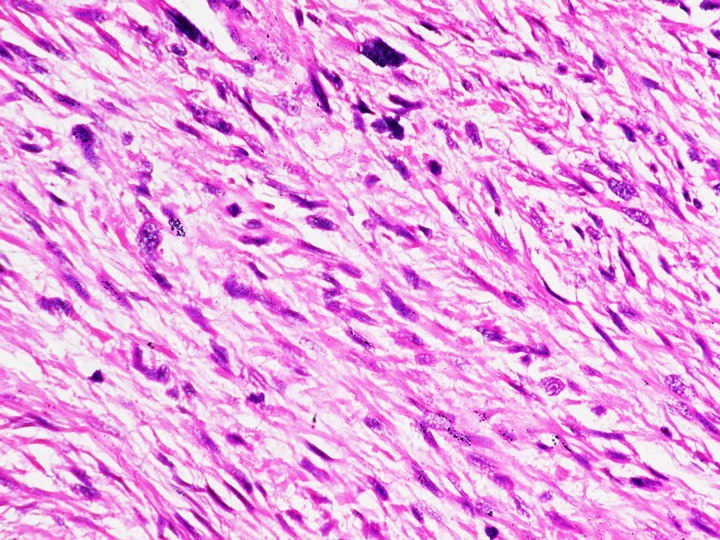
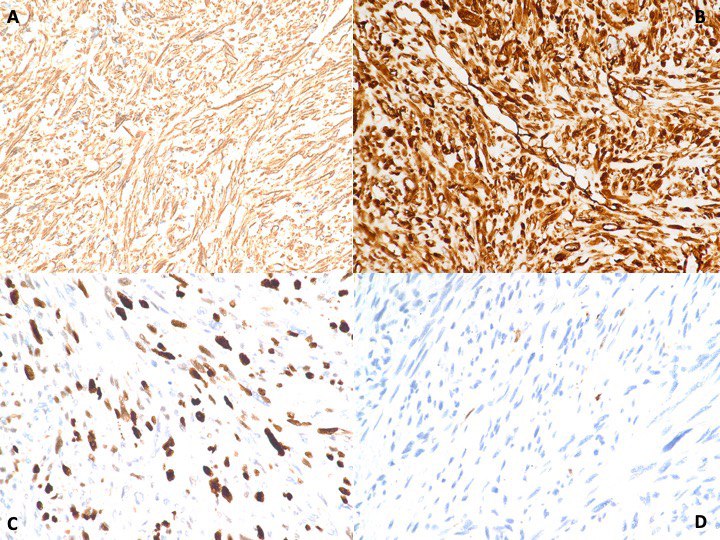
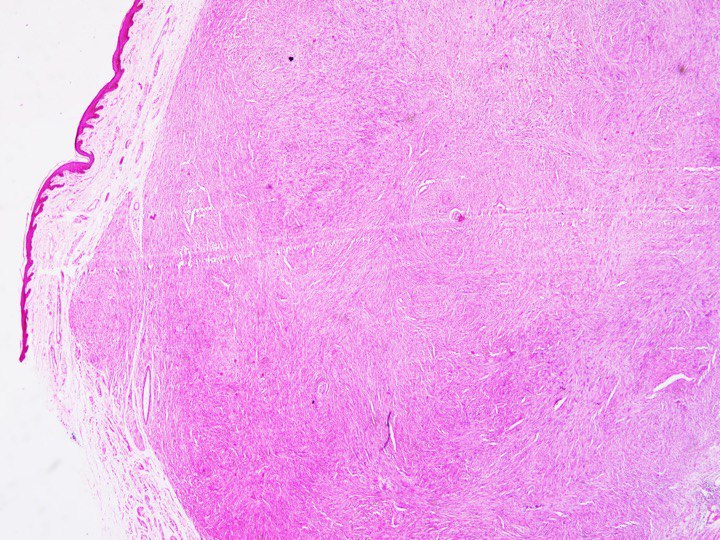
A 67 year old male, known case of type II diabetes mellitus, presented with thickening and difficulty in retraction of foreskin of penis for 08 months. This was associated with ballooning of foreskin and painful erections. Thickening of foreskin was insidious in onset and gradually progressive. There was no history of discharge per urethra, fever, burning micturition or hematuria. There was no history suggestive of sexually transmitted illness. On local examination, penis was central in position and urethra meatal opening was visible. The preputial skin was non retractable and showed a tender nodular thickened area measuring 1.5x1cm over its dorsal surface. All the haematological and biochemical blood parameters of the patient were well within normal limits. The patient underwent circumcision. Gross examination of the specimen received revealed a skin covered tissue measuring 4.5x2x0.8cm. A whitish circumscribed and non-encapsulated nodule was noted beneath the skin surface measuring 1.1x0.7x0.6cm. Cut surface of the nodule showed homogenous firm whitish area with no evidence of necrosis or haemorrhage. Microscopic examination of the nodule showed a well circumscribed lesion in the dermis exhibiting proliferation of atypical spindle cells arranged in short fascicles in a collagenous to myxoid background. Interspersed slit-like blood vessels are noted. Individual atypical spindle cells showed moderate nuclear pleomorphism, hyperchromatic cigar shaped nuclei, prominent nucleoli, and eosinophilic cytoplasm. Brisk mitosis was noted. No areas of necrosis was seen [Figure 1, Figure 2]. Immunohistochemistry performed revealed that the lesion was positive for Vimentin, SMA, Desmin, Caldesmon and was negative for CD34 and S100. Ki67 was 55% in the most proliferative areas [Figure 3]. Based on the above findings, a diagnosis of Cutaneous Leiomyosarcoma (atypical smooth muscle tumor) of prepuce (confined to dermis) was offered. However, the resected margin was less than 01 mm from tumour. In view of this, revision of circumcision margins was performed. A whole-body PET scan done showed no evidence of residual tumor. Presently, patient is stable and on follow up in oncology outpatient department of our hospital.
Figure 1
Haematoxylin & Eosin (H&E, 100X) section shows a skin lined tissue with anunencapsulated, partially circumscribed spindle cell tumour seen in the dermis.
Discussion
cLMS is a rare sarcoma of skin. The typical presentation of cLMS is small nodule over trunk and lower extremities in an elderly male. In our case, the tumour presented as a painful nodular lesion of prepuce. Such cases can go clinically undiagnosed due to the rarity of presentation. Literature review shows only two other case reports of cLMS of prepuce in the last 10 years. 6, 7 Prompt histopathological examination can clinch the diagnosis. The exact pathogenesis is still uncertain. However, leiomyoma and previous local trauma are considered as predisposing factors. Overexpression of receptor tyrosine kinases like IGFR and PDGFR have been reported. Dermal leiomyosarcoma is thought to arise from arrector pili muscle whereas subcutaneous leiomyosarcoma arises from vascular smooth muscle cells. 3 cLMS is clinically indistinguishable from benign cutaneous leiomyoma. Microscopically, cLMS is a well differentiated sarcoma of smooth muscle origin. They show increased cellularity with relatively uniform spindle cells disposed in fascicles having perinuclear vacuoles, cigar shaped nuclei and brisk mitotic figures. The presence of infiltrative pattern, high cellularity and brisk mitosis favours features of high-grade malignancy and excludes benign leiomyoma. Further, characteristic immunohistochemistry positivity for Vimentin, Desmin and Caldesmon confirms the diagnosis of cLMS over other spindle cell tumors. IHC was useful to exclude differential diagnosis considered such as Malignant peripheral nerve sheath tumor, Spindle cell melanoma, Synovial sarcoma, Spindle cell carcinoma, Fibrosarcoma and vascular tumors. The extensive panel of IHC including S100, SOX10, EMA, TLE1, PanCK and CD34 were all negative in our case. Marked nuclear pleomorphism and necrosis are generally absent in cLMS. The presence of these features is usually seen in cutaneous metastasis of extracutaneous LMS. 8 Hence, in presence of these microscopic features in cLMS, a thorough workup of patient is essential to rule out metastasis from an extracutaneous site. Patients having cutaneous metastasis from extracutaneous site have very poor prognosis with about 16 months of mean survival after metastasis. 4 A comparison of 62 case reports of penile leiomyosarcoma shows that the age of presentation ranges between 26 to 84 yrs, with majority of cases reported in 4th to 5th decades. The most common site of involvement was penile shaft followed by glans and prepuce. Circumcision scar was also rarely involved. cLMS showed heterogenous clinical presentation such as painless nodule, localized painful swelling and skin ulceration. Uncommonly, the tumor can invade the urethra causing hematuria. 4 Queiros et al, in a retrospective study of 20 years, compared 11 cases of cLMS. It was observed that most of the cases were elderly males with age at presentation ranging between 47 to 92 years. Head and neck were the most frequent location of tumor. There were no prepucial tumors reported. More than 60% of patients presented with painless nodule and rest were asymptomatic. Microscopically, majority were dermal leiomyosarcoma with only one case of extracutaneous leiomyosarcoma and all these cases were positive for SMA with variable positivity for Desmin and Vimentin.3 Our case is also in agreement with these observations. In cases of cLMS, it is mandatory to incorporate the precise location or penetration depth of lesion in skin in histopathology report for prognostication. Ours was a case of dermal cLMS which has better prognosis than subcutaneous LMS. In view of this, the nomenclature atypical smooth muscle tumours is suggested for cLMS rather than sarcomas. Pathological grading is not of prognostic value according to latest WHO classification of skin tumours. However, there are multicentric retrospective studies which have found strong association between higher risk of local recurrence or distant metastasis with histological features like higher tumour grade, poor tumour differentiation and high mitotic index. 9 The paucity of data on cLMS compared to deep soft tissue LMS is a limitation in studying the prognosis, staging and molecular genetics of cLMS. 1 All superficial LMS should undergo primary microscopically controlled surgery to achieve R0 resection with subsequent safety margin.10 Hence, in our case, the initial margin of 01 mm was rightly revised after the histopathology diagnosis to attain safety margin of 01 cm.
Conclusion
cLMS (atypical smooth muscle tumour) is a malignant mesenchymal tumour of elderly males. Although they generally have good prognosis, they have varying clinical behaviour based on its exact location. Owing to its rarity, index of clinical suspicion is usually low. Hence, precise histopathological examination supplemented by ancillary immunohistochemistry studies is diagnostic and essential in these cases. Favourable outcomes are seen if R0 resection is achieved with appropriate safety margins. Our case highlights the unusual presentation of a rare tumour and the role of microscopic examination and immunohistochemistry in its prompt diagnosis.