Introduction
Clear cell carcinoma of minor salivary gland is a very rare and a low grade malignant neoplasm. It represents approximately 1% of all salivary gland tumors and 0.2% of minor salivary glands.1 They are characterized by an indolent growth and less aggressive behavior. Clear cell carcinoma is more common in women and generally presents in fifth to eighth decade of life. They frequently occur in salivary glands in intra-oral region, like palate or tongue but can occur at other sites like skin, neck, thyroid gland, ear, jaw, etc.
Clear cell carcinoma is a diagnosis of exclusion as clear cells can be seen in various other neoplasms.2 Here, we describe a rare case of clear cell carcinoma of palatine minor salivary gland.
Case Report
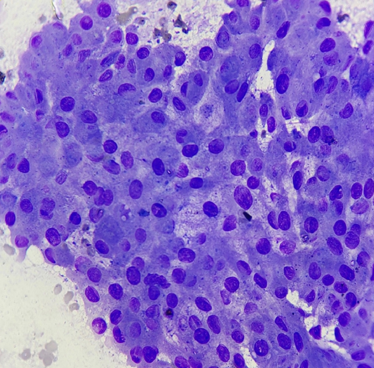
A 32-year-old female presented with painful swelling in the oral cavity for three months. On fine needle aspiration cytology, a diagnosis of SUMP (Salivary gland neoplasm of uncertain malignant potential) was given according to Milan Classification. [Figure 1] On examination, the patient was found to have a 3x3 cm soft cystic swelling on the left side of the hard palate and it was immobile. Neck nodes were not palpable. A contrast-enhanced computed tomography scan showed a soft tissue mass with internal non-enhancing necrotic areas measuring 2.6x1.9x1.6cm involving left upper alveolar mucosa with destruction of underlying maxillary bone and invading into the maxillary sinus. Patient underwent left side partial maxillectomy with obturator placement and skin grafting.
On histopathological examination, a final diagnosis of clear cell carcinoma was given with the tumour invading the maxillary bone and showing perineural invasion.
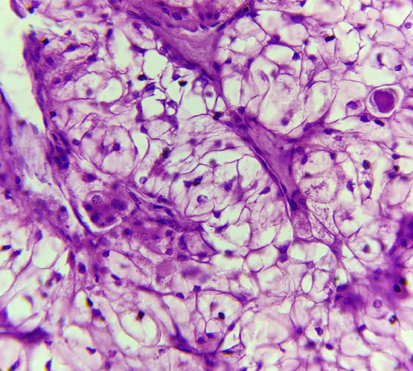
Grossly, the tumour was poorly circumscribed, solid and grey white, measuring 2.2x1.5x1.2 cm. [Figure 2, Figure 3]
Microscopically, the tumour showed sheets and nests of polygonal cells with clear cytoplasm and round to irregular nuclei. [Figure 4]
Discussion
Clear cell carcinoma (CCC), also known as clear cell carcinoma, not otherwise specified (NOS), of the salivary gland is a rare and low-grade malignant tumour. The first case of hyalinising clear cell carcinoma (HCCC) of the salivary gland was reported in 1994.3 It comprises less than 1% of all malignant tumors in the salivary glands. The majority (90%) of such cases occur predominantly in the minor salivary gland, which account for about 10% of all salivary gland tumors. The most commonly affected sites are the tongue and palate (50%). Our case was derived from the tumour in minor salivary gland of the palate.4, 5, 6 In a study conducted by Buchner et al., it was reported that more than 60% of HCCC occurred in middle-aged women over 50 years old, and the tumour size measured less than 2 cm in the greatest dimension in more than 55% of cases.7 Contrary to the above study, our patient was of younger age group and the greatest dimension of the tumour was more than 2 cm. According to the old WHO classification, clear cell carcinoma (NOS) of salivary gland included hyalinising clear cell carcinoma (HCCC), clear cell adenocarcinoma, and glycogen-rich adenocarcinoma.4, 5 However, in the revised WHO classification 2005, epithelial malignant tumors of salivary glandwith clear cell morphology are together categorized as clear cell carcinoma (NOS) and are not subtyped.5 Histopathological features of hyalinising clear cell carcinoma are as follows: (1) invasive proliferation of tumour cells organized in trabeculae, cords, or irregular solid nests surrounded by hyalinizing stroma in the perilesional tissue of salivary glands and (2) tumour cells with clear cytoplasm and round or polygonal nuclei.8, 9, 10
However, clear cell carcinoma (NOS) has been considered a diagnosis of exclusion,2 as clear cells can be found in various other tumors of salivary gland, such as epithelial myoepithelial carcinoma, mucoepidermoid carcinoma, acinar cell carcinoma, and metastases from renal cell carcinoma.9, 10 Immunohistochemistry (IHC) can be done to differentiate these tumours when needed. Clear cell carcinoma show positive expression for cytokeratin and p63, along with lack of expression of S100 and SMA. Epithelial myoepithelial carcinoma is a biphasic malignant tumour with inner duct like epithelial component and an outer myoepithelial component which will be S100+. Muco-epidermoid carcinoma will show variable amount of mucin, epidermoid and intermediate cells and will show mucicarmine positivity. Acinic cell carcinoma will have acinar structure and show less clear cells in comparison to clear cell carcinoma. Acinar cells in such tumours will be positive for DOG-1 and SOX-10. In renal clear cell carcinoma, the tumour cells will show co-expression of PAX-8, vimentin and CD10. In our case, ultrasound was done to rule out possibility of renal cell carcinoma. It is important to differentiate clear cell carcinoma from other tumors with clear cell morphology, as their treatment and clinical outcome differ.10
Complete local resection and follow up is considered the recommended treatment of clear cell carcinoma. A study has also shown a significant therapeutic effect by CDDP and 5-FU combination chemotherapy.6 Since less data is available, the efficacy of radiation therapy and chemotherapy has been controversial. It is said that this therapy should be chosen only for cases with postoperative recurrence or positive tumour resection margins. In cases of tumors with intra-oral origin, close proximity of tumour with the surgical resection margins can be particularly challenging, therefore surgical reconstruction may be required to prevent facial wounds and scar formation. Our patient underwent left side partial maxillectomy with obturator placement and skin grafting. No adjuvant chemotherapy or radiotherapy was given and the patient recovery is satisfactory with no local recurrence.
Conclusion
Clear cell carcinoma (CCC) of the minor salivary gland is an exceptionally rare and low-grade malignancy, often presenting a diagnostic challenge due to its overlapping histological features with other neoplasms. The case reported here highlights the importance of considering CCC in the differential diagnosis of intra-oral lesions, especially when clear cell morphology is observed. Comprehensive diagnostic approaches, including histopathological evaluation and immunohistochemical studies, are crucial for accurate diagnosis. Surgical resection remains the primary treatment modality, with careful follow-up necessary to monitor for recurrence. Given the rarity of this condition, further research and accumulation of case studies are essential to enhance our understanding and management of CCC of the minor salivary gland.