Introduction
Primary Central Nervous System malignant melanoma is a very rare disease. It represents only about 1% of all malignant melanomas and approximately 0.05% of all the primary brain tumors. 1
Melanomas can occur in any part of the body that contains melanocytes. However, it usually develops in the skin, mucosa, and choroid layer of eyes. In the central nervous system (CNS), melanocytes normally exist in the leptomeninges located on the inferior surface of the cerebrum and, the anterolateral surface of the brainstem and the spinal cord.2 Melanocytic lesions of CNS include melanomatosis, melanocytosis, melanocytomas and malignant melanoma. Leptomeningeal melanoma, also known as carcinomatous meningitis occurs secondary to the dissemination of cancer cells into the pia-arachnoid meninges. Melanocytosis and melanomatosis involves diffusely leptomeninges and superficial brain parenchyma and these are benign. Melanocytoma is a solitary, benign and low-grade tumor that occurs mostly in the intradural extramedullary cervical or thoracic spine.3 Malignant melanoma is a highly aggressive tumor with a poor prognosis, which arises from the melanoblasts.4 Secondary or metastatic intracranial malignant melanoma is frequent in patients with disseminated melanomas. However, primary intracranial leptomeningeal melanomatosis, also known as a meningeal variant of primary intracranial malignant melanoma is rare. Its rarity may contribute to the high chance of misdiagnosis, especially in the cases without skin lesions.5 Here, we report a rare case of primary leptomeningeal melanoma.
Case Report
A 47 year male presented in casualty with complain of forgetfullness, difficulty in walking, urinary incontinence since 20 days, along with complaints of drowsiness, unable to speak, seizure and vomiting. He was referred to our institute with above complaints and with MRI finding which showed altered signal intensity area with hemorrhagic component seen in right temporal lobe right insular region. Post Contrast study shows prominent gyral and parenchymal enhancement in lesion suggestive of possibility of hemorrhagic neoplasm, sol 64 x 31 x 47 mm diffuse meningeal thickening and enhancement is seen in basal cisterns. Bilateral sylvian fissures and along interhemispheric falx. Hemorrhagic component is seen in fourth ventricle, foramen of luscha and magendie. Severe Hydrocephalus seen in lateral ventricles.
For that, patient was operated for right side VP shunt and right frontotemporoparietal craniotomy with excision of right temporal space occupying lesion.
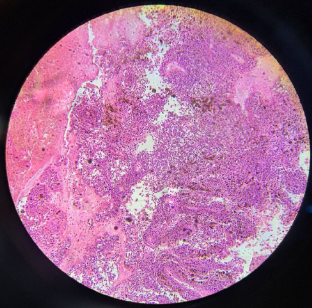
Gross examination
Specimen consists of brownish to blackish soft tissue portion measuring 4 x 3.5 cm in aggregate.
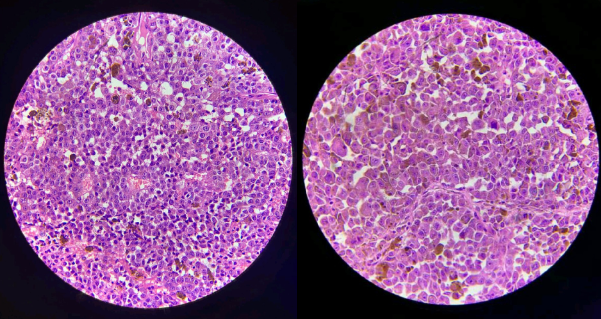
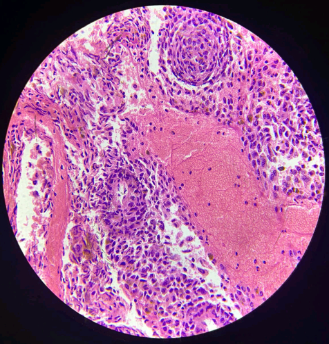
Microscopic examination
Histologically it is characterized by an intrusion of neoplastic cells arranged in sheets, nests and pentheliomatous pattern. Cells are epitheliod to spindly in nature with hyperchromatic, pleomorphic and vesicular nuclei with prominent nucleoli. Mitosis are (20/10 HPF). Cytoplasm of neoplastic cells showed melanin pigment. No evidence of necrosis is seen.
Immunohistochemistry report
IHC Marker:
MITF - Positive
HMB45 - Positive
SOX10 - Positive
KI 67 LABELLING INDEX IS 25-30%
IHC was done outside the institute.
Overall findings were reported as Leptomeningeal malignant melanoma.
Discussion
Leptomeningeal metastasis is defined as the appearance of tumor cells in the leptomeninges or CSF distant from the site of a primary tumor.6 It may originate from melanocytes or neural crest derived cells and more specifically from leptomeningeal melanocytes which reside in leptomeninges, or from meningeal melanoblasts which are precursor cells that may differentiate into melanocytes and may be the origin of LMM.7
The non-specific symptoms can occur like headache, mental status changes, confusion, dementia, seizure, hemiparesis.8 It is not taken into consideration against chronic subdural hematoma due to its very low incidence and non specific presentation.9 The specific symptoms include headache, often due to increased Intracranial pressure, patient is confused and feels sleepy all the time, has seizures and symptoms of meningitis. Spinal symptoms may include radicular pain that radiates to leg through spine, abnormal sensation of skin like tingling, pricking, chilling, burning, numbness, bowel or bladder dysfunctions, and limb weakness.10
Systemic cancer most commonly involving Leptomeningeal melanoma are breast cancer, followed by non small cell lung cancer and melanoma.11 CNS involvement is seen clinically in 25 to 30% of patients with melanoma and as high as 70 to 75% at autopsy.12 The tumor cell pathway to the meninges can be different in which the most common form of spread is mainly hematogenous followed by lymphatics, direct, choroid, de novo and iatrogenic. The basilar cisterns and cauda equina are most affected areas. 13
Differential diagnosis of LMM includes leptomeningeal lymphoma, meningeal melanocytoma, leptomeningeal carcinomatosis, leptomeningeal sarcomatosis, leptomeningeal glioma, metastasis from other primary sites such as RCC and thyroid carcinoma, also some inflammatory conditions such as chronic meningitis, sarcoidosis, vasculitis, etc.14 LMM can be differentiated from these differentials by clinical presentation and medical history, imaging studies (CT, MRI), CSF analysis, biopsy, and IHC (eg : S-100, HMB-45, Melan -A) to support melanocytic origin of LMM. 15
Conclusion
Primary CNS melanoma is a rare disease and when leptomeninges are involved, it has poor prognosis.
IHC report done outside institute shows tumor was focally positive for MITF, HMB45, SOX10 and KI 67 LABELLING INDEX was 25-30%.
Although clinicopathologic features may lead to diagnosis of leptomeningeal malignant melanoma (LMM), it is necessary to differentiate LMM with other differentials, due to its rare presentation.