Introduction
Chromoblastomycosis is a chronic fungal infection of the skin and subcutaneous tissue1 caused by pigmented or dematiaceous fungi, first described by Max Rudolph in 1914.2 The most common etiological agents are Fonsecaea pedrosoi, Fonsecaea compacta, Cladophialophora carionni and Phialophora verrucosa.3,4 The inoculation of infection usually follows after penetrating traumatic injury by thorn or splinter wounds. The fungal agents develop as small clusters of cells known as muriform bodies. Several months after the injury, painless papules or nodules appear in the affected area progressing to scaly and verrucose plaques.4 Most cases of fungal sinusitis have been due to aspergillosis or candidiasis.5 Here we report a rare case of maxillary chromoblastomycosis.
Case Report
A 34 years old Indian farmer presented with nasal discharge and epistaxis for the last 15 days. There was no swelling of the nasal dorsum or history of nasal trauma. Anterior rhinoscopy revealed multiple polyps in bilateral nasal cavities arising from maxillary sinuses along with blackish necrotic areas. Nasal mucosa, nasal septum and turbinates were unremarkable. Excision of bilateral polyps was done and sent for histopathological examination.
Pathology
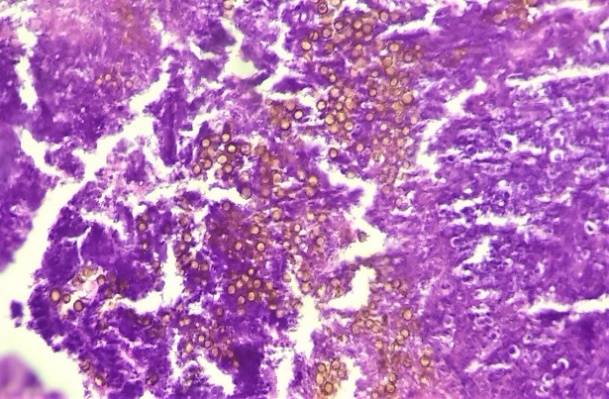
Macroscopically, the specimen of the polyps consisted of multiple fragmented pieces of grey white to grey brown glistening soft tissue with small remnants of blackish material. Microscopic examination of the formalin fixed paraffin embedded sections stained with H and E showed areas of necrosis with fungal elements composed of dark brown, round to oval sclerotic bodies of about 10 microns in size which were morphologically resembling chromoblastomycosis and also was a pathognomonic of chromoblastomycosis. These sclerotic bodies are also known as “ copper-pennies ”, “medlar bodies” or muriform cells. Other microscopic foci showed polypoidal lesions with extensive neutrophilic infiltrate, edema, granulation tissue and haemorrhage.
A culture of the subspecies was not done as the diagnosis of mycosis was not suspected at the time of surgery and the specimen was routinely fixed in formalin.
Conclusion
Chromoblastomycosis is a chronic localized infection of the skin and subcutaneous tissue predominantly affecting lower extremities following a trauma.2 It is more common in outdoor workers like farmers and forest workers.6 Unusual extracutaneous sites include pleural cavity, ileocecal region, laryngotracheal area and tonsils.7 Dissemination of infection although rare, presents with multiple verrucous nodules and plaques over limbs, neck, face, lymph glands and tonsil according to reports.8 The most frequent complication is secondary bacterial infection and rarely malignancies have also been documented.9
Chromoblastomycosis of sinuses are very rare and are usually mistaken for granulomatous conditions. In our case the disease was confined to maxillary sinuses and presented as nasal polyps, such cases may cause nasal obstruction, epistaxis or nasal discharge. It may be challenging to make the diagnosis of chromoblastomycosis clinically. The differentials of verrucous variants of tuberculosis, sporotrichosis and leishmaniasis may be considered.
Culture is done for identification of species, but is a slow process and can be inconclusive at times. Culture should be observed for a period of 3 weeks to 30 days as fungal agents are typically slow growing and culture may be inconclusive due to poor morphological differentiation. Polymerase chain reaction is also useful for species identification and can supplement culture when culture is inconclusive.10,11 It is a rapid and sensitive investigation and is widely available in the majority of centers. ELISA is another investigative tool, which is less commonly used but useful in monitoring response to long-term treatment.12